Standard Spinal Anaesthesia Then Turned Prone for Lower Limb Orthopaedic Surgeries
Nissar Shaikh, Mohamed Alkhayarin, AR Raju Vegesna and Syed Imran Ghouri
DOI10.21767/2471-982X.100021
Hamad Medical Corporation, Doha, Qatar
- *Corresponding Author:
- Nissar Shaikh, MD, EDIC
Hamad Medical Corporation, Doha, Qatar
Tel: 0097455320214
E-mail: nissatfirdous99@gmail.com
Received date: September 21, 2017; Accepted date: March 14, 2018; Published date: March 26, 2018
Citation: Alkhayarin M, Shaikh N, Ghouri SI, Vegesna ARR (2018) Standard Spinal Anaesthesia Then Turned Prone for Lower Limb Orthopaedic Surgeries. Int J Anesth Pain Med. Vol.4 No.1:4
Copyright: © 2018 Alkhayarin M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Spinal anesthesia compared to the general anesthesia has advantages of decrease blood loss, better cardiovascular stability and post-operative pain control. But the spinal anesthesia for lower limb orthopedic surgeries in prone position is not well described in the literature. The aim of this study was to know the safety and feasibility of spinal anesthesia for lower limb orthopedic surgeries in prone position.
Patients and Methods: Patients undergoing lower limb orthopedic surgeries in prone position under spinal anesthesia in a tertiary health care facility over a period of 10 years were included in this study. Patient demographic data, surgical procedure, ASA grade, position for spinal anesthesia, local anesthetic with or without opioids, level of sensory block and complication if any were recorded retrospectively.
Results: A total 104 patients were included in our study. The Majority of our patients were male. Fifty two percent had fracture calcaneus surgery. Average height of spinal block was thoracic 9 vertebra. Patients turned to prone position after 8.59 ± 3.6 minutes. Eighty seven percent patients received fentanyl with heavy bupivacaine. The most frequent complication was hypotension (18.3%). There were significant difference between occurrence of complication and patients age, gender, BMI, ASA grading and comorbid condition. No major complications occurred which needed to turn the patient back in to supine after prone positioning.
Conclusion: Spinal anesthesia and prone position is safe and feasible for lower limb orthopedic surgeries. Our study showed that complications of lower limb orthopedic surgeries in prone position under spinal anesthesia were negligible.
Keywords
Hypotension; Lower limb orthopedic surgery; Prone position
Introduction
Lower limb orthopedic surgeries in prone position are commonly performed under general anesthesia, but it had various hemodynamic and postural complications [1]. Not much literature is available about these surgeries under spinal anesthesia. There are few publications about emergency pilonidal surgeries in spinal anesthesia in prone position [2]. There are no publications about lower limb and foot surgeries under spinal anesthesia given in lateral or sitting position and then turning these patients to prone position for surgery.
The Aim of this study was to know feasibility and safety of lower limb and foot orthopedic surgeries under spinal anesthesia done in standard position and then turning patient to prone position for surgeries.
Patients and Methods
This study was done at tertiary health care facilities, after obtaining permission from institutional department of medical research and ethics. All patients underwent lower limb orthopedic surgery during Jan 2005 to 2014 under spinal anesthesia in prone position were included in the study, their records were reviewed retrospectively.
Patients demographic data, diagnosis, surgical procedure, position for spinal anesthesia, level of spinal anesthesia, time to turn the patient to the prone position, requirement of adjuvant general anesthesia, bradycardia, hypotension, nausea vomiting were recoded.
Spinal anesthesia was given in lateral or sitting position at the level of L4-5, with 2 to 2.5 ml of 5% heavy bupivacaine, with or without fentanyl. When used, the dose of fentanyl was 20 micrograms, mixed with bupivacaine; once sensory level was determined, and stable hemodynamically, patients’ position was changed to the prone for the surgical procedure. We made it a point not to turn the patient to the prone position till the blood pressure is stabilized for 5 minutes. Patients with local site infection, pediatric and pregnant patients were excluded from the study. Bradycardia was defined as heart rate less than 50/ minute.
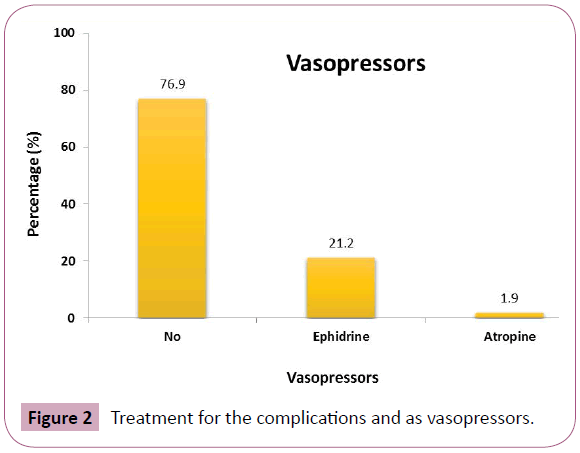
Hypotension is defined, when the systolic blood pressure dropped below 90 mm of Hg. Vasopressor used was ephedrine in incremental dosages of 3 mgs, total maximal dose of 30 mgs. Data entered on SPSS program, chi-square test and student t test was used to compare between groups. Any P value less than 0.05 was considered as significant.
Results
A total of 104 patients were included in this study. Majority of our patients were male. Mean age, height and weight was 35 ± 10.1 years, 1.672 ± 0.06 meters and 69.39 ± 13 kilograms. Majority of our patients (58.7%) belonged to the ASA1 category of anesthesia grading; only 3 patients were from ASA3 grade.
Fifty two percent patients had calcaneum fracture, 66.3% patients were healthy without any comorbid conditions and common comorbidity was combination of diabetes mellitus and hypertension (16.4%). Eighty five percent of patients had spinal anesthesia in the sitting position and 87.5% patients received fentanyl along with local anesthetic (Table 1). Patients were turned to the prone position after 8.59 ± 3.6 minutes, sensory blocked level was thoracic vertebral level 9 and duration of the surgery was 92.07 ± 61.15 minutes (Table 1).
| Characteristics | Mean ± SD [median (min-max)] N (%) |
| Age (years) | 35.1 ± 10.1 [33 (16-71)] |
| Height (m) | 1.672 ± 0.657[1.680(1.5-1.9)] |
| Weight (kg) | 69.39 ± 13.00[69.0(42-100)] |
| BMI | 24.70 ± 3.64[24.65 (16.40-32.74)] |
| Level of sensory block | 9.45 ± 1.16[10(5-12)] |
| Duration of Surgery (minutes) | 92.07 ± 61.15[72.5(10-360)] |
| Turned Position after (minutes) | 8.59 ± 3.60[8(3-19)] |
| IV fluids ( ml) | 1275 ± 523[1200(100-3000)] |
| Gender Male Female |
94 (90.3) 10 (10.7) |
| ASA 1 2 3 |
61(58.7) 40(38.5) 3(2.9) |
| Position for spinal Sitting Lateral |
88(84.6) 16(15.4) |
| Intrathecal Opioid Use Yes No |
91(87.5) 13(12.5) |
| Type of Surgery Calcaneal Tendo achilles Others |
55(52.9) 42(40.4) 7(6.7) |
| Associated Disease None Diabetes (DM) Hypertension (HTN) DM and HTN Smokers DM+HTN+Obesity Others |
69(66.3) 1(1.0) 6(5.8) 2(1.9) 17(16.3) 5(4.8) 4(3.8) |
| Complications No Yes |
80(76.9) 24(23.1) |
Table 1: Demographic, anaesthetic, surgical and clinical characteristics of the patients.
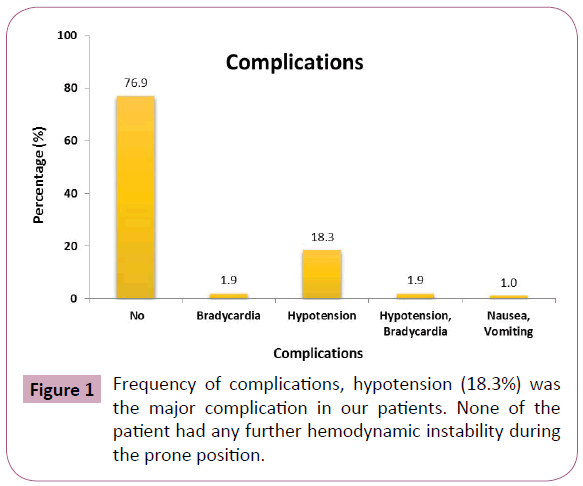
When the complications were concerned in our study; there was no significant difference in occurrence of complications according to age, BMI (body mass index), comorbidities, ASA grading, duration for prone positioning (Table 2). There were fewer complications in patient who did not receive opioid with local anesthetics (Table 2). All these complication after the spinal anesthesia occurred in supine position; no patient required changing to supine position once prone position is given due any reasons. Figure 1 shows the frequency of complications, hypotension (18.3%) was the major complication in our patients. None of the patient had any further hemodynamic instability during the prone position. Figure 2 is showing treatment for the complications and as vasopressors is required by 21.3% of our patients.
| Variable | Complication (n=24) | No complication (n=80) | p-value |
| Age (years) | 37.8 ± 10.6 | 34.3 ± 9.9 | 0.142 |
| BMI (mean ± SD) | 24.3 ± 4.0 | 24.8 ± 3.6 | 0.517 |
| Gender | 21 (22.8) | 71 (77.2) | 0.612 |
| Male | 3 (30.0) | 7 (70) | |
| Female | |||
| Turned Position after (minutes) | 9.38 ± 3.70 | 8.34 ± 3.56 | 0.223 |
| Duration of Surgery (minutes) | 99.63 ± 52.16 | 89.80 ± 63.72 | 0.493 |
| IV fluids – ml | 1332.61 ± 493.05 | 1258.75 ± 533.84 | 0.554 |
| Co-morbidity | 0.73 | ||
| None | 17 (24.6) | 52 (75.4) | |
| DM, HTN, HTN & DM | 0 (0) | 9 (100) | |
| Smokers | 4 (23.5) | 13 (76.5) | |
| DM, HTN & Obesity | 2 (40) | 3 (60) | |
| Others | 1 (25) | 3 (75) | |
| ASA | |||
| 1 | 15 (24.6) | 46 (75.4) | 0.791 |
| 2 | 8 (20) | 32 (80) | |
| 3 | 1 (33.3) | 2 (66.7) | |
| Opioid Used | |||
| No | 5 (38.5) | 8 (61.5) | 0.159 |
| Yes | 19 (20.9) | 72 (79.1) | |
Table 2: Association of various related factors with complications.
Discussion
Surgeries under spinal anesthesia have distinct advantages of decreased blood loss, the decrease in perioperative cardiac ischemic incidents, post-operative hypoxic episodes, arterial venous thrombosis and better postoperative pain control [3]. It also prevents ophthalmic, fascial and upper limb injuries during general anesthesia [4]. But there is not much literature available about safety of spinal anesthesia in prone position for orthopedic surgeries. In this study after spinal anesthesia patients were positioned into prone for lower limb orthopedic surgeries.
Chang et al. also compared the spinal anesthesia for supine and prone position surgeries using isobaric bupivacaine, there was no significant difference in sensory & motor block level [5]. Our study was having higher patient sample and we used hyperbaric bupivacaine. Average height of sensory blocked in our patients was at thoracic 9th dermatome. We were meticulously monitoring the sensory level by using alcohol swab and adjusting the patients’ position to avoid higher sensory block.
Mehmet et al compared hyperbaric and isobaric bupivacaine for spinal anesthesia with reference to the hemodynamic and heart rate variability, and they concluded that hyperbaric bupivacaine had significantly lesser heart rate variability and hemodynamic instability [6].
The common complication of the spinal anesthesia is hypotension, due to the sympathetic blockade; the incidence of hypotension in our study was 18.3% and it was the major complication in our patients, without any other serious cardiovascular events. In literature the reported occurrence of the post spinal hypotension varies from 5 to 56% [7].
There are various risk factors for the occurrence of post spinal hypotension such as advanced age, female gender, hypovolemia, pregnancy, obesity, diabetes mellitus, hypertension and anemia. In our study the incidence of post spinal hypotension was comparable to that of mentioned in the literature [8].
Conclusion
This study shows that complications of spinal anesthesia and prone position for lower limb orthopedic surgeries were comparable. The Lower limb orthopedic surgeries in prone position under spinal anesthesia are feasible and safe.
References
- Tetzlaff JE, O’Hara Jr JF, Yoon HJ, Schubert AS (1998) J Clin Anaesthesia 10: 656-659.
- Larsen JR (1997) Emergency spinal anaesthesia in prone position. Acta Anesth Scand 40: 790-791.
- Attari MA, Mirhosseini SA, Hornarmand A, Safavi MR (2011) Spinal anaesthesia versus general anaesthesia for elective lumbar spine surgery: a randomised clinical trial. J Res Med Sci 16: 524-529.
- Shruti C, Hardman JG (2006) Injury during anesthesia. Continuing Education in Anesthesia Critical Care & Pain Volume 6: 67-70.
- Chang CH, Namy T, Jeong JY, Choi SI, Lee YW (2003) Comparative study of Isobaric bupivacaine spinal anaesthesia in supine and prone position. Korean J anesthesiol 44: 605-611.
- Toptas M, Uzman S, Isitemiz I, Uludag Yanaral T, et al. (2014) A comparization of effects of hyperbaric and isobaric bupivacaine spinal anaesthesia on hemodynamic and heart rate variability. Turk J Med Sci 44: 224-231.
- Klasen J, Junger A, Hartmann B, Benson M, Jost A, et al. (2003) Different incidence of revelent hypotension with combined spinal epidural anaesthesia and spinal anaesthesia. Anesth Analg 96: 1491-1495.
- Bren CK, Hartmann B, Katzer C, Obaid R, Bruggmann D, et al. (2009) Hypotension after spinal anesthesia for caesarean section: identification of risk factors using anaesthesia information management system. J Clin Moni Comput 23: 85-92.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences