Anesthetic Challenges and Management of a Gravid Achondroplastic Dwarf
Afsheen Nasir, Anum Mughal and Safia Zafar Siddiqui
DOI10.21767/2471-982X.100024
Afsheen Nasir, Anum Mughal* and Safia Zafar Siddiqui
Department of Anaesthesiology, SiCU and Pain management, Civil hospital Karachi, Sindh, Pakistan
- *Corresponding Author:
- Anum Mughal
Post graduate trainee at Department of Anaesthesiology
SICU and pain management, Civil Hospital karachi, Sindh, Pakistan.
Tel: +923343544989
E-mail: anum_leo@hotmail.com
Received date: May 07, 2018; Accepted date: June 21, 2018; Published date: June 29, 2018
Citation: Nasir A, Mughal A, Siddiqui SZ (2018) Anesthetic Challenges and Management of a Gravid Achondroplastic Dwarf. Int J Anesth Pain Med. Vol.4 No.1:7
Copyright: © 2018 Nasir A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Achondroplasia, the most common form of human chondrodysplasias, is a rare disorder of impaired endochondral bone ossification, observed in 1/20,000 live births, as a result of over activation of fibroblast growth factor receptor 3 (FGFR3), a tyrosine kinase receptor that restrains over-proliferation of chondrocytes. The ensued mutation in the FGFR3 and its signaling results in various skeletal anomalies. The cause of skeletal dysplasia is frequently a de-novo mutation; however, the mode of inheritance is autosomal dominant if a parent carries a mutated FGFR3 gene. The homozygous form is fatal and has characteristics comparable to thanatropic dwarfs. Supervision of pregnancy in achondroplastic patients is a demanding task for obstetricians owing to cephalo-pelvic abnormalities and spinal curvature disorders. Furthermore, the airway anomalies create an impediment in the anesthetic management of such patients, including laryngomalacia, sternal protuberance, pulmonary malformations, cervical instability, inflexible temporomandibular joint and obstructive sleep apnea; therefore stringent preoperative assessment is obligatory. We reported an anecdotal case of a 28-year-old achondroplastic gravid woman who was referred to us from a tertiary care unit at 33 weeks of gestation. Frequent follow-up appointments with obstetrician, cardiologist, and anesthesiologist were performed due to the escalated risk of various complications. A comprehensive prenatal counseling, extensive assessments of potential risks were conducted by a multidisciplinary team to design a multiparametric management plan. The patient underwent general anesthesia following the failure of spinal anesthesia induction for an emergency caesarean section. We elucidate the risk-benefit analysis associated with the administration of regional and general anesthesia in achondroplastic parturients. The case offers an insight into devising a systemic management plan for such patients undergoing anesthesia induction. The dilemmas in anesthetic management are also emphasized.
Keywords
Achondroplasia; Dwarfism; Anaesthetic regional; Difficult airway; General anaesthesia; Anaesthesia spinal
Introduction
Achondroplasia is the most common skeletal dysplasia caused by the gain-of-function mutations in fibroblast growth factor receptor 3 (FGFR3) gene [1,2]. 80% mutations are the result of sporadic mutations while 20% are inherited in an autosomal dominant fashion. Linkage analyses in achondroplastic patients demonstrated a gene localized to 4p 16.3, resulting in the substitution of an arginine residue for a glycine residue (G380R), leading to FGFR3 over activation [1]. FGFR3 is a negative regulator of chondrocyte proliferation, the exact molecular mechanism in humans remains elusive [3]. Over-expression of FGFR3 signaling, a tyrosine kinase receptor, results in diminished chondrocyte proliferation in the epiphyseal growth plate [4]. Moreover, in-vitro experimental studi es in transgenic mice and chondrocytes acquired from thanatropic and achondroplastic dwarfs demonstrated a defect in primary ciliary (PC) functions owing to the perturbed signaling of intraflagellar trafficking 20 (IFT 20) proteins to PC [5]. The characteristic clinical features include rhizomelia, midface hypoplasia, and skeletal deformities [6]. Moreover, reduced functional residual capacity (FRC) of the lungs, spinal stenosis, and spinal curvature disorders make them high-risk candidates for anesthetic management. Therefore, a multidisciplinary team of obstetrician, pulmonologist, cardiologist, otolaryngologist, and anesthesiologist should follow such patients with a meticulous peripartum assessment, preferably in a preoperative testing center.
Case Report
A 28-year-old, gravid 1/para 0, achondroplastic female was admitted to the hospital for an elective cesarean section in virtue of cephalopelvic disproportion (Figure 1). She presented at 33 weeks’ gestation complaining of exacerbating dyspnea since six months of pregnancy. The physical examination demonstrated an amicable patient who was 92 cm tall and weighed 77 lbs (Table 1). She had a normal-sized face, short neck, depressed anteroposterior diameter of the chest, distended abdomen with splayed lower ribs. Upon mouth opening, soft-palate and uvula were noticeable (Modified Malampatti class III). Back examination demonstrated notable spinal scoliosis and lumbar lordosis. Lower limb examination revealed a valgus deformity and talipes varus of the left limb along with motor dysfunction. The chest was clear to auscultation bilaterally with an audible early systolic murmur at the apex of the heart. Electrocardiography (ECG) was normal; Echocardiography revealed left ventricular dysfunction, mild aortic and mitral valve regurgitation, and mild pulmonary artery hypertension. Her blood reports, electrolytes, renal function tests, were within normal limits respectively. Ultrasonography demonstrated a viable fetus.
| Height | 92 cm |
| Weight | 35 kg |
| Diabetic evaluation | HbA1c 7.0% |
| Renal status | Urea 17, Cr 0.9 |
| Cardiac profile | Ejection fraction >55% Mild MR, mild AR Mild pulmonary HTN |
| Pulmonary function test | NA |
Table 1: The physical examination.
The patient was recruited to the operating room. During the discussion of the different anesthetic options with the patient, she requested to remain awake during the surgery; therefore, regional anesthesia was given first. A 25 gauge spinal needle was placed at L4-L5 interspace, and 8 mg of 0.5% hyperbaric bupivacaine was injected. The outcome of spinal anesthesia resulted in unilateral numbness, hence administration of general anesthesia was proposed. Following proper positioning and preoxygenation with 100% oxygen, rapid sequence induction with intravenous propofol 2 mg/kg and succinylcholine 1.5 mg/kg was done. After 45 seconds, direct laryngoscopy was performed which revealed the tip of the epiglottis (Cormack Lehane classification: grade III) exclusively. An intubating bougie was introduced under the epiglottis; as the bougie approached the cricoid rings, an endotracheal tube (ETT) of 6.0 mm internal diameter was railroaded over the bougie into the trachea. The fixation of ETT was confirmed by auscultation and capnography. A left manual uterine displacement technique was performed. Anesthesia maintenance was done with 4 liters of oxygen, isoflurane 0.6 volume %, and atracurium 0.1 mg/kg infused at regular intervals, while nalbuphine 0.1 mg/kg was injected for analgesia after the delivery of the baby.
An alive male baby weighed 2.5 kg, with the APGAR score of 6 in 1 minute and 8 in 5 minutes, was delivered. Rest of the procedure went uneventfully without any anesthetic and surgical complications respectively. At the end of a procedure, the transverse abdominis plane (TAP) block was injected for analgesia.
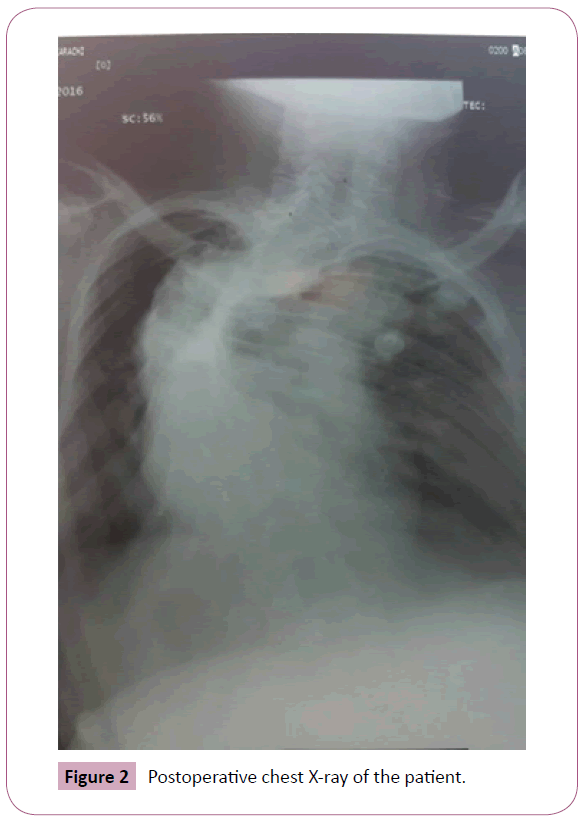
Postoperative chest X-ray of the patient showed marked dextroscoliosis obliterating both lung fields and significant deviation of trachea towards the right side (Figure 2). The patient was extubated 4 hours post-surgery and was kept under observation and managed accordingly. The perioperative course was uneventful.
Discussion
The most common mode of delivery in achondroplastic patients is an elective cesarean section due to pelvic abnormalities [7]. The selection of administering general or regional anesthesia in such patient is crucial because of various skeletal deformities, however, the decision of utilizing general over spinal anesthesia or vice-versa remains elusive, as apparent by a handful of case studies. The challenges encountered during the induction of general anesthesia include difficult mask ventilation owing to macroglossia, poor dental occlusion, difficult fixation of the mask due to the flat nasal bridge, rigid temporomandibular joint, inability in neck extension, and atlanto-occipital joint instability [7,8]. Kyphoscoliosis in these patients jeopardizes cardiac and respiratory functions, leading to cardiorespiratory compromise and failure [7,9]. Moreover, superimposed physiologic changes in pregnancy including enlarged breast, airway edema, upper airway capillary engorgement, aortocaval compression due to a gravid uterus, expanded plasma volume and increased consumption of oxygen can considerably complicate the state of health of such patients [10].
The obstacles encountered during the administration of regional anesthesia include the unpredictable spread of local anesthetic agent as a result of spinal stenosis and hyper lumbar lordosis in supine position [11]. Modero et al. demonstrated no notable complications in airway management with spinal anesthesia [12]. Besides, some reports demonstrated favorable outcomes in securing the airways with regional anesthesia, including spinal [13], epidural [14], and combined spinal and epidural [15] respectively. Trikh et al. preferred combined spinal-epidural (CSE) technique over spinal or epidural technique.
In our patient, the failure of regional anesthesia ensued as a consequence of spinal stenosis. In spite of the narrowed airway and pre-existing cardiac concerns, general anesthesia administration demonstrated commendatory outcomes. Our objective was to elucidate preoperative complications encountered in such patients along with contemplating the pros and cons of administrating general or regional anesthesia on a case to case basis. Besides, a multitude of problems in such patients necessitates a careful pre-anesthetic evaluation to warrant patients' safety and affirmative outcomes.
Declaration
Conflict of interest
The authors declare that they have no competing interests.
Authors’ contribution
Afsheen Nasir and Anum Mughal did manuscript drafting and critically review the manuscript. Both authors finalize and agree on final Draft. Both authors read and approved the final manuscript.
References
- Shiang R, Thompson LM, Zhu YZ, Church DM, Fielder TJ, et al. (1994) Mutations in the transmembrane domain of FGFR3 cause the most common genetic form of dwarfism, achondroplasia. Cell 78: 335-342.
- Segev O, Chumakov I, Nevo Z, Givol D, Madar-Shapiro L, et al. (2000) Restrained chondrocyte proliferation and maturation with abnormal growth plate vascularization and ossification in human FGFR-3(G380R) transgenic mice. Hum Mol Genet 9: 249-258.
- Qi H, Jin M, Duan Y, Du X, Zhang Y, et al. (2014) FGFR3 induces degradation of BMP type I receptor to regulate skeletal development. Biochim Biophys Acta 1843: 1237-1247.
- Aviezer D, Golembo M, Yayon A (2003) Fibroblast growth factor receptor-3 as a therapeutic target for Achondroplasia--genetic short limbed dwarfism. Curr Drug Targets 4: 353-365.
- Martin L, Kaci N, Estibals V, Goudin N, Garfa-Traore M, et al. (2017) Constitutively-active FGFR3 disrupts primary cilium length and IFT20 trafficking in various chondrocyte models of achondroplasia. Hum Mol Genet 27: 1-13.
- Langer LO, Baumann PA, Gorlin RJ (1967) Achondroplasia. AJR Am J Roentgenol 100: 12-26.
- Kuczkowski KM (2003) Labor analgesia for the parturient with an uncommon disorder: a common dilemma in the delivery suite. Obstet Gynecol Surv 58: 800-803.
- Mather JS (1966) Impossible direct laryngoscopy in achondroplasia. A case report. Anaesthesia 21: 244-248.
- Bergofsky EH, Turino GM, Fishman AP (1959) Cardiorespiratory failure in kyphoscoliosis. Medicine (Baltimore) 38: 263-317.
- Beilin Y, Leibowitz AB (1993) Anesthesia for an achondroplastic dwarf presenting for urgent cesarean section. Int J Obstet Anesth 2: 96-97.
- Jeong ST, Song HR, Keny SM, Telang SS, Suh SW, et al. (2006) MRI study of the lumbar spine in achondroplasia. A morphometric analysis for the evaluation of stenosis of the canal. J Bone Joint Surg Br 88: 1192-1196.
- Monedero P, Garcia-Pedrajas F, Coca I, Fernandez-Liesa JI, Panadero A, et al. (1997) Is management of anesthesia in achondroplastic dwarfs really a challenge? J Clin Anesth 9: 208-212.
- DeRenzo JS, Vallejo MC, Ramanathan S (2005) Failed regional anesthesia with reduced spinal bupivacaine dosage in a parturient with achondroplasia presenting for urgent cesarean section. Int J Obstet Anesth 14: 175-178.
- Rudas OW, Garcia NIS, Upegui A, Medina AR, Moran A, et al. (2012) Anestesia para cesárea en paciente con acondroplasia. Revista Colombiana de Anestesiología 40: 309-312.
- Trikha A, Goyal K, Sadera GS, Singh M (2002) Combined spinal epidural anaesthesia for vesico-vaginal fistula repair in an achondroplastic dwarf. Anaesth Intensive Care 30: 96-98.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences