Bilateral Occipital Phenol Neurolysis
Kalpana R Kulkarni
Kalpana R Kulkarni*
D.Y. Patil Medical College & Hospital, Kolhapur (Maharashtra), India
- Corresponding Author:
- Dr. Mrs. Kalpana R Kulkarni
1168, a-5, “chaitanya”, takala square
Kolhapur- 416008 (Maharashtra) India
Tel: 9822065665
E-mail: drrmk@rediffmail.com
Received Date: September 09, 2015, Accepted Date: October 27, 2015, Published Date: November 04, 2015
Abstract
Background: Occipital neuralgia is a condition of severe paroxysms of burning; shock like pain in the distribution of occipital nerves and often confused with other causes of headache syndromes like migraine or cluster headache. Relief with local anesthetic block off occipital nerves have a significant diagnostic value.
Case study: A 35 years old female presented with history of episodes of severe shock like, burning pain in suboccipital, frontoparietal region bilaterally and occasionally in retrobulbar region with neck stiffness since one year. She failed to respond to the conservative management, hence given local anesthetic block with steroid of occipital nerves bilaterally on two occasions followed by neurolytic block with phenol at interval of one month. There was reduction in VAS from 9 to <2 at the end of three months. Oral analgesics and anticonvulsants were continued for one month and tapered off over 15 days. On follow up at 6 months and one year she was comfortable with VAS < 2 and no analgesic support needed.
Conclusion: Occipital nerve block with local anesthetic is a diagnostic as well as safe and simple therapeutic option for the relief of occipital neuralgia. Phenol induced neurolysis can be an effective method for long term relief.
Keywords
Neuropathic pain; Bi-lateral occipital nerve block; Chemical neurolysis
Introduction
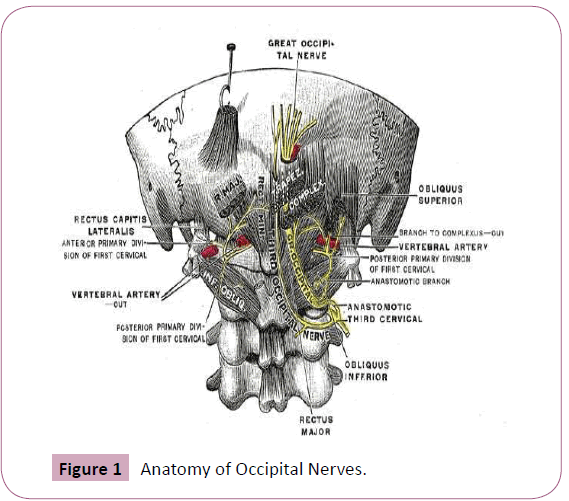
Occipital neuralgia is a condition characterized by paroxysms of stabbing/shooting pain in suboccipital region that radiates over vertex in the dermatomes of nervus occipital major in 90% or minor in 10% and both in 8.7%. Mostly it is unilateral but can be bilateral, associated with dysasthesia/parasthesia and pain on palpation and often difficult to differentiate from other headache syndromes. The greater occipital nerve receives sensory fibers from C2 and lesser occipital nerves from C2 and C3 nerve roots. It develops due to entrapment of the nerves in trapezius and semispinalis capitis muscles at the attachment to occipital bone (Figure 1). Local anesthetic blocks of occipital nerves at periphery or at C2/C3 roots are helpful for diagnosis [1-3]. Other treatment modalities are medications, nerve blocks with steroids/Botox, Radio Frequency (RF) ablation of occipital nerves or surgical interventions [4,5].
Case Study
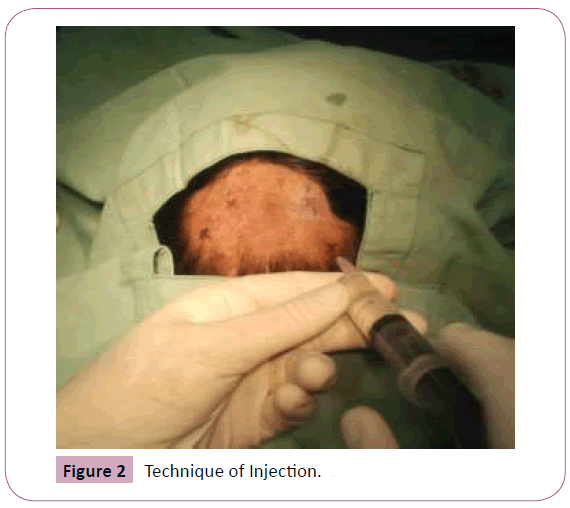
A 35 years old lady presented with severe throbbing, burning pain in posterior part of the head bilaterally radiating to frontoparietal and occasionally retrobulbar region, that increased since 1 month. It was associated with neck pain and stiffness. The attacks were paroxysmal lasted for 4-8 hrs/4 days in a week initially, but then the frequency and duration was increased (VAS 8-9), inability to sleep and pain on touching the occipital area. There was no history of trauma/surgery. She was consulted and treated by neurophysician, orthopedician and psychiatrist over a year but failed to respond. Systemic examination was normal. Her blood investigations and CT head was normal. X-ray and MRI cervical spine showed spondylotic changes at C5-6, C6-7 level. Considering the urgency of treatment and nonavailability/affordability for RF treatment chemical neurolytic block of occipital nerves bilaterally was planned. Following Informed consent, diagnostic local anesthetic nerve block of greater and lesser occipital nerve was performed on both the sides. Oral diazepam 10 mg was given night before and Inj. glycopyrrolate 0.2 mg, Inj. diclofenac 75 mg was given intramuscularly 30 minutes prior to the procedure. Inside operation theater patient was given sitting position with head resting forward on the pillow over table. Vital monitoring started. The occipital artery pulsations palpated on the line joining the external occipital protuberance to mastoid process (superior nuchal line) approximately at a distance of 3 cm, a point marked just medial to the pulsations. Another point marked 2.5 cm below and lateral to the first point to block lesser occipital nerve which is lateral to the occipital artery (Figure 2). Under asceptic precautions with 27G needle local infiltration of the skin over the site at greater and lesser occipital nerves with 2% lignocaine 1 ml each was given on both the sides. A 22G needle introduced till bone contact occurred and parasthesia elicited. 2 ml of 0.5% bupivacaine injected at each site on one side first and then other. There was pain relief in 15-30 min and VAS score was <2 .The VAS score remained <3 but increased gradually at one month. The procedure repeated after 1 month with addition of triamcenolone 20 mg at each point. Third setting was given at 3rd month with neurolysis using 1 ml of 8% phenol at each site following 2 ml of 0.5% bupivacaine injection. No immediate or late complications reported following neurolytic block. Oral supplementation with gabapentine 400mg BID, Flupirtine Maleate 100 mg BID, duloxetine 40 mg and clonazepam 0.5 mg HS was given for 1 month later tapered over 15 days period. The pain relief was gradual and VAS reached <2 at 6 months.The last follow up was at one year when patient was comfortable without analgesic support. She was able to sleep on pillows which she was unable to do before the nerve blocks.
Discussion
Occipital neuralgia also known as Arnold’s neuralgia may be primary or secondary due to trauma/surgery, associated with cervical spondylosis, diabetic neuropathy, tumour infiltration. It resembles with migraine and other headache syndromes. The clinical diagnosis is based on symptoms and presence of dysasthesia or pain on palpation/pressure over suboccipital region and relief with occipital nerve blocks. Detailed neurological evaluation is needed to detect intracranial pathologies. CT head and MRI cervical spine helps to rule out other causes headaches, neck pain due to facet arthropathy, spondylosis etc. Association of dizziness, vertigo or hypertension with pain is known. Local anesthetic occipital nerve blocks are diagnostic and have short term therapeutic value [2,6]. Addition of Botulinum Toxin (botox) is found to relieve pain and muscle spasm for 4 months in patients with migraine and also reported to relieve other primary headache syndromes. It reduces the length, duration and severity of migraine so can be a treatment option for occipital neuralgia [5,7]. For prolonged effect neurolysis or dorsal root rhizotomy can be performed [8,9]. Fluroscopy or ultrasound guidance may be useful to improve the precision of nerve block [10]. Neurolysis of occipital nerves with alcohol/ phenol in glycerine or Omnipaque is a safe intervention to have prolonged effects [11]. Adverse effects are minimal like dizziness, light headedness or local tenderness. Care should be taken to avoid intravascular injection and local anesthestic toxicity. Rhizotomy is an invasive method of cutting the nerves but can result in dennervation pain. Ganglioneurectomy is more extensive procedure than rhizotomy, but observed to have short term pain relief of less than 3 months in 95% of patients in a study done by [12]. Currently, radiofrequency ablations of C2–C3 nerves are widely practiced over neurolysis. However denervation pain can develop with worst pain than before [13,14]. Pulsed radiofrequency of occipital nerves have promising results [1,4]. Surgical decompression is done for relief of resistant pain can be considered but it is invasive/ complex procedure. Ducic et al in his metaanalysis reported 86% success in patients who underwent surgical decompression [15]. Occipital nerve stimulation with implantable TENS has been studied for relief of pain with variable success and complication like lead migration is reported [16,17]. In the absence of RF ablation which would have been safer, but costly option for our patientwe offered alternative method of chemical neurolysis which is reported to have minimal risk of complications. In our patient VAS Score decreased with each successive nerve block and following phenol neurolysis oral medications were tapered with complete relief from neuralgic pain that lasted for one year and not yet reported for recurrence of pain.
Conclusion
The occipital nerve block is a valuable diagnostic and safe therapeutic intervention for occipital neuralgia. Phenol induced neurolysis can be considered as a safe option for longer effects if advanced modalities are not available.
Acknowledgement
I thank our D Y Patil Institution for the support to publish the case report.
References
- Headache Classification Subcommittee of the International Headache Society (2004) The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 24: 9-160.
- Hammond SR, Danta G (1978) Occipital neuralgia. Clin Exp Neurol. 15: 258-270.
- Afridi SK, Shields KG, Bhola R, Goadsby PJ (2006) Greater occipital nerve injection inprimary headache syndromes-prolonged effects from a single injection. Pain. 122: 126-9.
- Vanelderen P, Rouwette T, De Vooght P, Puylaert M, Heylen R, et al. (2010) Pulsed radiofrequency for the treatment of occipital neuralgia: a prospective study with 6 monthsof follow-up. Reg Anesth Pain Med. 35: 148-151.
- Blumfeld AM, Dodick DW, Silberstein SD (2004) Botulinum neurotoxin for the treatment of migraine and other primary headache disorders. Dermatol Clin. 22: 167-75.
- Vanelderen P, Lataster A, Levy R, Mekhail N, van Kleef M, et al. (2010) Occipitalneuralgia. Pain Pract. 10: 137-144.
- Freund BJ, Schwartz M (2002) Use of botulinum toxin in chronic whiplash-associated disorder. Clin J Pain. 18: S163-8.
- Bovim G, Fredriksen TA, Stolt-Nielsen A, Sjaastad O (1992) Neurolysis of the greateroccipital nerve in cervicogenic headache. A follow up study. Headache. 32: 175-179.
- Ward JB(2003) Greater occipital nerve block. Semin Neurol. 23: 59-62.
- Gray AT(2006) Ultrasound-guided regional anaesthesia: current state of theart.Anaesthesiology. 104: 368-73.
- SerdarErdine,Gobar B Racz,Carl E Noe.Somatic blocks: Head and Neck.P PrithviRaj. Interventional Pain Management: Image-Guided procedures. Sounders.p: 102.
- Acer F, Miller J, Golshani KJ, Israel ZH, McCartney S, et al.(2008) Pain relief aftercervical ganglionectomy (C2 and C3) for the treatment of medically intractable occipitalneuralgia.Stereotact Neurosurg. 86: 106-112.
- Hamer JF, TA Purath(2014) "Response of cervicogenic headaches and occipitalneuralgia to radiofrequency ablation of the C2 dorsal root ganglion and/or third occipital nerve."Headache 54: 500-510.
- Huang JH,Galvagno SMJr,Hameed M,Wilkinson I, Erdek MA, et al. (2012) "Occipital nerve pulsed radiofrequency treatment: a multi-center study evaluating predictors of outcome." Pain Med. 13: 489-497.
- Ducic I,Felder JM 3rd,Fantus SA(2014) "A systematic review of peripheral nerveinterventional treatments for chronic headaches." Ann Plast Surg. 72: 439-445.
- McGreevy K (2012) "Updated perspectives on occipital nerve stimulator leadmigration: case report and literature review." Clin J Pain. 28: 814-818.
- Weiner RL, Reed KL (1999) Peripheral neurostimulation for control of intractable occipital neuralgia. Neuromodulation. 2: 217-221.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences