Case Report: Anesthesia Management in a Male Patient Planned for Mastectomy under Thoracic Paravertebral Block
Deniz Turan and Serdar Epözdemir
DOI10.36648/2471-982X.21.7.41
Deniz Turan and Serdar Epözdemir*
Istanbul Medipol University Camlica Hospital, Anesthesia and Reanimation Clinic, Ä°stanbul, Turkey
- *Corresponding Author:
- Serdar Epözdemir
Istanbul Medipol University Camlica Hospital
Anesthesia and Reanimation Clinic
Ä°stanbul
Turkey
Tel: 5327798350
E-mail: epzdemir@yahoo.com
Received Date: March 23, 2021; Accepted Date: April 06, 2021; Published Date: April 13, 2021
Citation: Turan D, Epözdemir S (2021) Case Report: Anesthesia Management in a Male Patient Planned for Mastectomy Under Thoracic Paravertebral Block. Int J Anesth Pain Med Vol.7 No.3:41
Abstract
We can benefit from regional blocks in operations where general anesthesia is not suitable and the patient has a fear of general anesthesia. Especially with the widespread use of ultrasonography, the use of peripheral blocks is increasing, thus eliminating the risk of general anesthesia and ensuring that the patient is operated in a safe, comfortable and satisfied manner.
Keywords
Mastectomy; General anesthesia; Thoracic paravertebral block; Electrocardiography
Introduction
We can benefit from regional blocks in operations where general anesthesia is not suitable and the patient has a fear of general anesthesia. Especially with the widespread use of ultrasonography, the use of peripheral blocks is increasing, thus eliminating the risk of general anesthesia and ensuring that the patient is operated in a safe, comfortable and satisfied manner.
Since there was no ultrasonography in our clinic, we used a 22 gauge 100 mm nerve stimulator cannula (Stimuplex A, B Braun, Germany) accompanied by a nerve stimulator.
Case Presentation
Male patient of 57 years, 1.75 height and 85 kg weight, upon planning of left breast mastectomy by general surgery, she was directed to us. The patient, who had no additional disease, was evaluated by requesting routine hemogram, biochemical examinations, Electrocardiography, posterior anterior Chest Xray, and no abnormal findings were found. The patient had a history of smoking and alcohol use and no history of allergies.
During the preoperative evaluation, when the patient stated that he was afraid of general anesthesia and therefore did not want general anesthesia, we explained to the patient that this operation can be performed with the anesthesia method called paravertebral block, but that general anesthesia can be switched to if an unfavorable situation develops, and the necessary information about thoracic paravertebral block was transferred to the patient. After the patient accepted the procedure, the necessary surgical and anesthesia consent forums were obtained and a thoracic paravertebral block was planned as an anesthesia method.
Materials and Methods
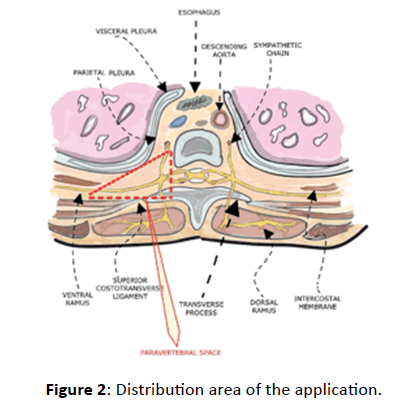
The patient was premedicated on the morning of the operation, 30 minutes before he was brought to the operating room, as an intravenous infusion with 3 mg of midazolam and 100 ml of saline. After the patient was taken to the operating room, he was monitored and his pulse, electrocardiography, heart rate, and oxygen saturation were recorded. For thoracic paravertebral block, the patient was given a sitting position, after aseptic conditions were provided, local anesthesia with 2% lidocaine was applied to the skin and subcutaneous tissues. At the thoracic 5th Vertebra (T5) level, with a 22 gauge 100 mm nerve stimulator cannula (Stimuplex A, B Braun, Germany) accompanied by a nerve stimulator (Stimuplex A, B Braun, Germany), after touching the transverse process at a depth of approximately 3 cm from the left lateral distance of 2.5 cm from the T5, the needle slightly It was retracted and advanced at an angle of 10 degrees towards the cephala, the upper edge of the transverse protrusion was crossed, the superior costotransverse ligament was detected by feeling the “pop”, stimulated by the nerve stimulator (2 milliampere, 0.3 millisecond, 1 Hz) Contractions were observed, then the current was reduced to 0.5 milliamperes.
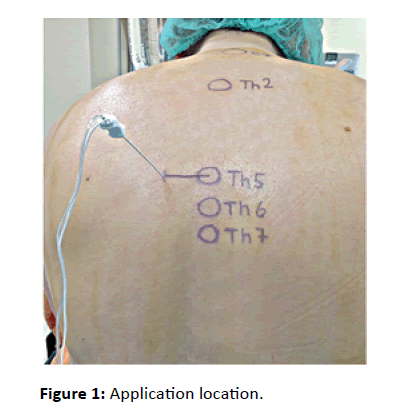
Upon the contractions continued, 20 ml of 0.5% Marcaine was applied in 5 ml each. The patient was placed in a normal supine position (Figure 1). When the patient's hemodynamics and general condition remained stable, 20 mg of intravenous anesthetic propofol was administered for sedation. After the necessary controls and tests were carried out, the surgical procedure was allowed to begin (Figure 2).
Results
Our patient is male, 57 years old, 1.75 height, 85 kg weight. The operation was initiated with blood pressure arterial: 130/80 mmHg, Pulse: 88 Beats/min, Oxygen Saturation (SpO2) 99. There was no problem during the operation, which lasted about 1 hour. Left mastectomy operation was successfully performed without the need for general anesthesia. The patient did not need additional analgesic postoperatively. The patient was transferred to the ward after being observed in the recovery unit for 30 minutes. No pain was observed for 7 hours in the service follow-up.
Discussion
Developments in the science of anaesthesiology in the modern world have gradually reduced traditional anesthesia methods in their application areas and made new anesthetic approaches obligatory. It is one of these methods in the Paravertebral Block. It is up-to-date in both intraoperative applications and postoperative pain control [1].
Thoracic Paravertebral Block (TPVB), which is accepted as an important component of malign surgical operations and postoperative pain management; It is often preferred because of its decreasing intraoperative opioid need and its perioperative analgesic properties. Adequate surgical anesthesia is provided with a single level of TPVB performed in mastectomy operations [2]. We believe that a good surgical anesthesia was provided after the block in our patient. Although general anesthesia is a technique that can be used in mastectomies, it alone does not provide sufficient postoperative pain control. Thanks to prolonged postoperative pain management with TPVB, it can be a good alternative to general anesthesia.
Pusch et al. [3,4] reported that a single injection of high volume into the thoracic paravertebral space is an effective anesthesia method for breast masses and axillary cleansing. Arunakul et al. stated that with TPVB performed together with general anesthesia, severe analgesia is provided in the first 24 hours postoperatively. A good clinical situation is expected due to prolonged postoperative analgesia [5]. Considering the longterm analgesic effect of single injection paravertebral block, this effect prolongs 12 hours according to some authors and up to 24 hours according to some authors. As a matter of fact, in our patient, it was observed that severe analgesia was provided in the first 8 hours postoperatively and intraoperatively after the block [6-8].
Conclusion
As a result, we conclude that Thoracic Paravertebral Block applications are a good choice in terms of both mastectomy operations and postoperative analgesia.
References
- Eason M J, Wyatt R (1979) Paravertebral thoracic block-a reappraisal. Anaesthesia 34: 638-642.
- Rukewe A, Afuwape OO, Ugheoke A, Fatiregun AA (2016) Single-shot lamina thoracic paravertebral block with ketofol for modified radical mastectomy. Local Reg Anesth 6: 83-86
- Sahu A, Kumar R, Hussain M, Gupta A, Raghwendra KH (2016) Comparisons of singleinjection thoracic paravertebral block with ropivacaine and bupivacaine in breast cancer surgery: A prospective, randomized, double blinded study. Anesth Essays Res 10: 655-660.
- Pusch F, Freitag H, Weinstabl C, Obwegeser R, Huber E, et al. (1999). Single-injection paravertebral block compared to general Osmangazi Medical Journal, March 2020 159 anaesthesia in breast surgery. Acta Anaesthesiol Scand 43: 770-774.
- Arunakul P, Ruksa A (2010) General anesthesia with thoracic paravertebral block for modified radical mastectomy. J Med Assoc Thai 93: 149-153.
- Tatiana S, Oreste B, Eleonora F, Beatrice MS, Georgia K, et al. (2008) A prospective comparison of continuous wound infiltration with ropivacaine versus singleinjection paravertebral block after modified radical mastectomy. Anesth Analg 106: 997-1001.
- Karmakar MK (2001) Thoracic paravertebral block. Anesthesiology 95: 771-780.
- Schnabel A, Reichl SU, Kranke P, PogatzkiZahn EM, Zahn PK (2010) Efficacy and safety of paravertebral blocks in breast surgery: A metaanalysis of randomized controlled trials. Br J Anaesth 105: 842-852.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences