Perioperative Critical Incidents in Pediatric Anesthesia at a Referral Hospital of Togo, Sub-Saharan Africa
Assenouwe Sarakawabalo1,2*, Mouzou E Tabana2,3, Tchagbele Ouro-Bagna2, Tchetike Pikabalo1, Sam- Awortwi Jnr Wilfred4, Poko Magnoudewa1, Sibabi-Akpo K Okassate5 and Lare Gnikimani1
1Department of Anesthesiology and Intensive Care, University Hospital of Lome, Lome, Togo
2School of Health Sciences, University of Kara, Kara, Togo
3Department of Anesthesiology and Intensive care, University Hospital of Kara, Kara, Togo
4College of Health Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
5Department of Pediatric surgery, University Hospital of Lome, Lome, Togo
- *Corresponding Author:
- Assenouwe Sarakawabalo
Department of Anesthesiology and Intensive Care, University Hospital of Lome,
Togo,
E-mail: sassenouwe@yahoo.fr
Received date: December 29, 2022, Manuscript No. IPAPM-23-15615; Editor Assigned date: January 02, 2023, PreQC No. IPAPM-23-15615 (PQ); Reviewed date: January 13, 2023, QC No. IPAPM-23-15615; Revised date: January 23, 2023, Manuscript No. IPAPM-23-15615 (R); Published date: January 31, 2023, DOI: 10.35841/2471-982X.9.1.87
Citation: Sarakawabalo A, Tabana ME, Ouro-Bagna T, Pikabalo T, Wilfred SAJ, et al. (2023) Perioperative Critical Incidents in Pediatric Anesthesia at a Referral Hospital of Togo, Sub-Saharan Africa. Int J Anesth Pain Med Vol.9 No.1: 87.
Abstract
Background and Aims: Pediatric anesthesia is associated with high morbidity and mortality, especially in low-income countries. Our study aimed to describe perioperative critical incidents and identify the associated factors.
Material and Methods: We conducted a prospective, observational cohort study from August 3 to November 3, 2020, including patients aged 15 years or younger. Intraoperative and early postoperative critical incidents were recorded. The Chi-square test was used for identifying morbidity factors.
Results: The study included 153 patients with a mean age of 6.27 ± 4.7 years and a sex ratio of 2.3. The procedure was emergent in 51.6% of cases. Patients were classified as ASA one in 76.5% and ASA ≥ 3 in 7.1%. Anesthesia was performed by nurse anesthetists alone in 75.2%. Critical incidents occurred in 49.0% of patients. Hypoxia (3.3%), hypotension (3.3%), difficult ventilation and intubation (2.0%) occurred during anesthesia induction. During the maintenance phase, there was hypoxia (4.6%), hypotension (4.6%), and shivering (3.3%). During recovery and postoperatively, delayed recovery (10.5%), hypoxia, and vomiting occurred in 2.6%, respectively. Six patients (3.9%) died postoperatively from acute respiratory distress syndrome (50.0%), septic shock, hemorrhagic shock, and ventilator failure in 16.7%, respectively. Age less than two years, emergent surgery, ASA class ≥ 3, and absence of an anesthesiologist were associated with the occurrence of critical incidents.
Conclusion: Respiratory and cardiovascular events are the common critical incidents in pediatric anesthesia. Age less than two years, emergent surgery, ASA class ≥ 3, and the absence of an anesthesiologist are associated with morbidity.
Keywords
Morbidity; Mortality; Critical incidents; Pediatric anesthesia; Perioperative
Introduction
Pediatric anesthesia has specificities related to the physiological, anatomical, pharmacological, and psychological peculiarities of children. It is associated with a higher risk of morbidity and mortality than adults [1,2]. The incidence of perioperative complications is ranged from 5.6% to 33.1%, and the mortality rate from 103 to 410 per 10,000 anesthetics. In developed countries, morbidity and mortality have decreased in recent decades, due to advanced anesthetic and surgical practices. However, in low-income and middle-income countries, it is still high. But few studies have assessed the risk factors for morbidity in these countries [3-10].
This study was designed to identify perioperative critical incidents in pediatric anesthesia and assess the risk factors.
Materials and Methods
Study design
This study was approved by the Ethical committee and authorized by the hospital director. Written informed consent was obtained from the parents or legal guardians of all patients before inclusion. Patient data were collected in compliance with ethical standards and in accordance with the principles of the declaration of Helsinki. We conducted a prospective, observational cohort study, from August 3 to November 3, 2020. Patients aged 15 years or younger, who underwent a procedure under anesthesia, were included. The anesthesia was provided by anesthesiologists, who were Anesthesia Attending Physicians (AAPs), and Nurse Anesthetists ( NAs) w ho graduated with a bachelor’s or Master's.
Data collection
Patients were selected during the pre-anesthetic visit for emergencies, and the day before the procedure for elective procedures. We recorded demographic characteristics, preanesthetic and intraoperative data, and critical incidents occurring intraoperatively and during the first 48 hours postoperatively, or until discharge prior 48 hours.
A perioperative critical incident was defined as any adverse event that complicated the normal course of anesthesia and altered the patient's vital signs during anesthesia or postoperatively.
Statistical analysis
Data were summarized as mean and Standard Deviation (SD) for continuous variables, frequencies and percentages for categorical variables. Statistical analysis was performed with Epi Info 3.5.4 software (Epi Info™, center for disease control and prevention, USA). The Chi-square test was used to study the association between critical incidents and the following clinical variables: Age, sex, American Society of Anesthesiologists (ASA) physical status, type of procedure, surgical specialty, anesthetic technique and anesthetist qualification. The statistical significance was defined as a P-value ≤ 0.05.
Results
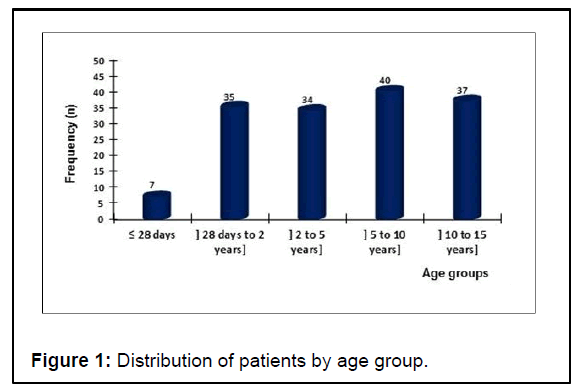
Our study included 153 patients aged 20 hours to 15 years, with a mean age of 6.27 ± 4.7 years (Figure 1). One hundred seven patients (69.9%) were males (sex ratio = 2.3).
The procedures were elective in 74 patients (48.4%), while 79 cases (51.6%) were emergencies. Patients underwent digestive (27.4%), urological (21.6%), trauma (17.6%), ear, nose and throat (16.3%), neurosurgical (7.2%), plastic (5.9%), and orthopedic (3.9%) procedures. A ter preoperative evaluation, 117 patients (76.5%) were categorized as ASA 1; 25 (16.3%) as ASA 2; 10 (6.5%) as ASA 3, and one (0.6%) as ASA 5.
General Anesthesia (GA) was used in 129 patients (84.3%) and spinal anesthesia in 24 patients (15.7%). Inhalational induction of GA was performed in nine patients (5.9%), Intravenous (IV) induction in 95 patients (62.1%) and both inhalational and IV induction in 25 patients (16.3%). The following anesthetics were used: Propofol (65 cases, 42.5%), fentanyl (41 cases, 26.8%), halothane (53 cases, 34.6%), sevo lurane (49 cases, 32.0%), iso lurane (16 cases, 10.5%), and rocuronium (six cases, 3.9%). Anesthesia was performed by NAs alone in 115 cases (75.2%) and both AAPs and NAs in 38 cases (24.8%). Intraoperative monitoring included Saturation of Peripheral Oxygen (SpO2) in all patients, an electrocardiogram in 148 patients (96.7%), noninvasive blood pressure in 147 patients (96.1%), the respiratory rate in 147 patients (96.1%), and capnography in 18 patients (11.9%). The mean duration of the surgery was 82 minutes ± 44 minutes.
One hundred and five critical incidents were recorded in 75 patients, with an incidence rate of 49.0%. Out of these, 82 (78.1%) occurred intraoperatively and 23 (21.9%) postoperatively. Sixty-two patients (40.5%) experienced one critical incident; nine patients (5.9%) experienced two critical incidents, and four patients (2.6%) experienced three critical incidents. Twenty-three patients (15.0%) experienced critical incidents during anesthesia induction (Table 1).`
| Frequency | Percentage | |
|---|---|---|
| Respiratory incidents | 17 | 11.1 |
| Difficult ventilation | 3 | 2 |
| Hypoxia* | 5 | 3.3 |
| Expected difficult intubation& | 3 | 2 |
| Esophageal intubation | 2 | 1.3 |
| Bronchospasm | 2 | 1.3 |
| Failure of laryngeal mask airway | 1 | 0.6 |
| Coughing upon intubation | 1 | 0.6 |
| Cardiovascular incidents | 6 | 3.9 |
| Hypotension | 5 | 3.3 |
| Shock | 1 | 0.6 |
| Total incidents | 23 | 15 |
| Note: *SPO2<95% for more than 30 seconds, not due to other respiratory events. &Intubation procedure that lasted more than 10 minutes and/or required more than three attempts. |
||
Table 1: Critical incidents recorded during induction period.
During the anesthetic maintenance period, 29 patients (19.0%) experienced critical incidents (Table 2).
| Frequency | Percentage | |
|---|---|---|
| Respiratory incidents | 8 | 5.2 |
| Hypoxia* | 7 | 4.6 |
| Laryngospasm | 1 | 0.6 |
| Cardiovascular incidents | 16 | 10.5 |
| Hypotension | 7 | 4.6 |
| Hypovolemic shock | 3 | 2 |
| Tachycardia | 3 | 2 |
| Bradycardia | 3 | 2 |
| Shivering | 5 | 3.3 |
| Total incidents | 29 | 19 |
| Note: *SPO2<95% for more than 30 seconds, not due to other respiratory events. | ||
Table 2: Critical incidents recorded during anesthetic maintenance period.
During emergence and postoperative periods, critical incidents occurred in 30 (19.6%) and 12 patients (7.8%) respectively (Table 3).
| Frequency | Percentage | |
|---|---|---|
| Emergence period | 30 | 19.6 |
| Delayed Awareness | 16 | 10.5 |
| Respiratory incidents | 9 | 5.9 |
| Hypoxia* | 4 | 2.6 |
| Apnea# | 2 | 1.3 |
| Stridor | 3 | 2 |
| General and miscellaneous incidents | 5 | 3.3 |
| Agitation | 3 | 2 |
| Vomiting | 2 | 1.3 |
| Postoperative period | 12 | 7.8 |
| Respiratory incidents | 7 | 4.6 |
| Hypoxia* | 4 | 2.6 |
| Stridor | 3 | 1.7 |
| Cardiovascular incidents | 6 | 3.9 |
| Tachycardia | 4 | 2.6 |
| Shock | 2 | 1.3 |
| General and miscellaneous incidents | 4 | 2.6 |
| Nausea/vomiting | 4 | 2.6 |
| Death | 6 | 3.9 |
| Note: *SPO2<95% for more than 30 seconds, not due to other respiratory events. #Apnea during sedation with spontaneous mask ventilation. |
||
Table 3: Critical incidents recorded during emergence and postoperative periods.
Six patients were declared dead postoperatively. The mortality rate was 3.9% (390 per 10,000 anesthetics). These six patients were categorized as ASA 3 (five cases; 3.3%) and ASA 5 (one case; 0.6%). All underwent an emergent procedure and died from acute respiratory distress syndrome (three cases: 50.0%), septic shock, hemorrhagic shock, and ventilator failure in one case (0.6%) respectively.
The occurrence of critical incidents was correlated with patient’s characteristics (Table 4), anesthetic and surgical characteristics (Table 5). These included: Age less than two years, emergent surgery, ASA class ≥ 3, and absence of an anesthesiologist during anesthetic management
| Total frequency (%) | Frequency of CI* (%) | Incidence (Frequency of CI*/total frequency) | p-value | |
|---|---|---|---|---|
| Total cases | 153 | 75 | 49 | |
| Age | 0.0001 | |||
| ≤ 28 days | 7 (4.6) | 6 (8.0) | 85.7 | |
| [28 days-2 years] | 35 (22.9) | 26 (34.7) | -74.3 | |
| [2 years-5 years] | 34 (22.2) | 15 (20.0) | 44.1 | |
| [5 years-10 years] | 40 (26.1) | 18 (24.0) | 45 | |
| [10 years-15 years] | 37 (24.2) | 10 (13.3) | 27 | |
| Sex | 0.23 | |||
| Male | 107 (69.9) | 55 (73.3) | 51.4 | |
| Female | 46 (30.1) | 20 (26.7) | 43.5 | |
| Note: *CI = Critical Incidents | ||||
Table 4: Patients characteristics associated with the occurrence of critical incidents.
| Total frequency (%) | Frequency of CI* (%) | Incidence (Frequency of CI*/total frequency) | p-value | |
|---|---|---|---|---|
| Type of procedure | 0.002 | |||
| Emergency | 79 (51.6) | 48 (64.0) | 60.8 | |
| Elective | 74 (48.4) | 27 (36.0) | 36.5 | |
| Surgical specialty | 0.503 | |||
| Digestive | 42 (27.4) | 26 (34.7) | ||
| Urology | 33 (21.6) | 15 (20.0) | 45.4 | |
| Traumatology | 27 (17.6) | 10 (13.3) | 37 | |
| ENT# | 25 (16.3) | 13 (17.3) | 52 | |
| Neurosurgery | 11 (7.2) | 5 (6.7) | 45.4 | |
| Plastic | 9 (5.9) | 4 (5.3) | 44.4 | |
| Orthopedic | 6 (3.9) | 2 (2.7) | 33.3 | |
| ASA class | 0.006 | |||
| 1 | 117 (76.5) | 53 (70.7) | 45.3 | |
| 2 | 25 (16.3) | 11 (14.7) | 44 | |
| 3 | 10 (6.5) | 10 (13.3) | 100 | |
| 5 | 1 (0.6) | 1 (1.3) | 100 | |
| Anesthetic technique | 0.734 | |||
| General anesthesia | 129 (84.3) | 64 (85.3) | 49.6 | |
| Spinal anesthesia | 24 (15.7) | 11 (14.7) | 45.8 | |
| Anesthetic team | 0.035 | |||
| AAP&present | 38 (24.8) | 13 (17.3) | 34.2 | |
| AAP&absent | 115 (75.2) | 62 (82.7) | 53.9 | |
| Note: *CI=Critical Incidents | ||||
| #ENT=Ear, nose and throat surgery | ||||
| &Anesthesia attending physicians (anesthesiologists) | ||||
Table 5: Anesthetic and surgical characteristics associated with the occurrence of critical incidents.
Discussion
In this prospective study, we recorded critical incidents during pediatric anesthesia in a tertiary hospital. The anesthetic and surgical characteristics were analyzed to identify factors associated with the occurrence of critical incidents. Our study indicated that pediatric surgery involved all age groups, from birth to 15 years. Critical incidents were frequent, especially during the intraoperative period.
Most patients in our cohort (92.8%) were categorized as ASA 1 or 2. The ASA physical status was similar to that reported in previous studies [2,4-9,11-13]. Indeed, children are growing individuals who rarely have comorbidities or impaired vital conditions; as a result, their ASA status is relatively healthy.
The incidence rate of critical incidents is heterogeneous based on the study designs and anesthesia safety in each country. The incidence reported in our cohort was higher than that reported in most studies. In 2013, a previous survey in our hospital reported 12.3% of perioperative incidents [5]. Amengle AL in Cameroon and Akodjènou J in Benin reported, respectively, 33.1% and 23.7% [6,7]. This difference may be due to the design and objectives of these previous studies. They were designed retrospectively or aimed to describe the practice of pediatric anesthesia. Therefore, critical incidents could be underreported.
In middle-income and high-income countries, the incidence rate is ranged from 0.5% to 5.2% [2,11,14]. This suggests inadequate anesthetic safety for pediatric anesthesia in our study. Indeed, most of the anesthesia cases were performed by non-physician anesthetists, and monitoring was insufficient. The lack of monitoring has been reported in sub-Saharan African countries [7,12,15].
Respiratory events were the most common critical events during the induction period, whereas cardiovascular events were more frequent during the anesthetic maintenance period. These results were in line with those reported in the literature [2,6,11,16]. Respiratory events were mostly related to airway control, including ventilation and intubation, awareness, recovery of spontaneous ventilation, and the extubation process.
Delayed awakening was the most common incident during the emergence phase, with an incidence rate of 10.5%. This incident is frequent in low-resource countries, with an incidence ranging from 1.3% to 15.5% [4,6]. It’s high frequency could be attributed to the pharmacology of anesthetic drugs used in these countries, as well as other adverse events like hypothermia and hypotension, which increased the risk of delayed recovery [17]. Halothane, isoflurane, and fentanyl were the most commonly used anesthetic drugs for maintenance in these countries [4-6,12,15].
These drugs have the worst hemodynamic adverse effects and slower elimination [18,19].
The anesthetic management in our study resulted in a high mortality rate. All deaths occurred during the postoperative period. This high mortality results from difficulties in surgical management, anesthesia, and pediatric resuscitation. In lowresource countries, many challenges have been identified: The insufficiency of anesthesiologists, particularly those specialized in pediatric anesthesia; the scarcity of centers specializing in pediatric surgery; the difficulties in accessing consumables and medicines; and the low income of patients [15,20,21].
The morbidity factors identified in our study were similar to those reported previously [5,22-25]. Furthermore, in our study, the absence of an anesthesia-attending physician was found to be a perioperative morbidity factor. A similar result was reported by N'guessan YF [26].
Our results suggest that pediatric anesthesia needs to be improved by training specialized anesthetists, especially anesthesiologists; creating specialized centers for pediatric surgery and pediatric intensive care units; improving the technical platform; and ensuring the availability of the safest medicines.
Limits of Our Study
There are some limitations to this study:
• This was a monocentric study whose results could differ from other centers. Thus, extension to all pediatric surgical centers could be limited.
• The short study period did not allow meeting all known critical incidents.
Conclusion
Pediatric anesthesia involves patients with ASA classes 1 and 2 in most cases. The incidence of critical incidents is high. Respiratory incidents predominated during the induction period, and cardiovascular incidents were most common during the maintenance period. Age less than two years, emergency surgery, ASA class 3 and above, and the absence of anesthesiologists are the main morbidity factors. Improvements in anesthesia and intensive care staff training, anesthetic equipment, consumables, and drugs would reduce morbidity and mortality.
Funding
No funding was received to assist with the study and the preparation of this manuscript.
Conflicts of interest
The authors have no relevant financial or non-financial interests to disclose.
Acknowledgment
The authors would like to thank Tekpor Esse for the statistical analysis.
References
- Bunchungmongkol N, Somboonviboon W, Suraseranivongse S, Vasinanukorn M, Chau-in W, et al. (2007) Pediatric anesthesia adverse events: The thai anesthesia incidents study (Thai Study) database of 25,098 cases. J Med Assoc Thai 90: 2072–2079.
[Google Scholar], [Indexed]
- Habre W, Disma N, Virag K, Becke K, Hansen TG, et al. (2017) Incidence of severe critical events in paediatric anaesthesia (APRICOT): A prospective multicentre observational study in 261 hospitals in Europe. Lancet Respir Med 5: 412-425.
[Crossref], [Google Scholar], [Indexed]
- De Graaff JC, Johansen MF, Hensgens M, Engelhardt T (2021) Best practice and research clinical anesthesiology: Safety and quality in perioperative anesthesia care. Update on safety in pediatric anesthesia. Best Pract Res Clin Anaesthesiol 35: 27-39.
[Crossref], [Google Scholar], [Indexed]
- Ogondon B, Cesar PYD, Koffi N, Yapi N, Abhe CM, et al. (2014) Pratique de l’anesthesie pediatrique en urgence au CHU de Cocody (Abidjan-RCI). Rev Afr Anesthesiol Med Urgence 19: 31-35.
- Mouzou T, Egbohou P, Tomta K, Sama H, Assenouwe S, et al. (2016) Pratique de l’anesthesie pediatrique dans un pays en developpement: Experience du CHU Sylvanus Olympio de Lome au Togo. Rev Afr Anesthesiol Med Urgence 21: 38-43.
- Amengle AL, Bengono R, Metogo Mbengono JA, Zambo A, Esiene A, et al. (2020) Complications per et postoperatoires en anesthesie pediatrique dans 2 hopitaux de reference du Cameroun. Rev Afr Anesthesiol Med Urgence 25: 16-21.
- Akodjenou J, Mewanou S, Ahounou E, Laleye Y, Zoumenou E, et al. (2021) Practice of pediatric anesthesia in Sub-Saharan Africa: Experience of two referral hospitals in benin. Journal of Pediatrics 7: 219-224.
- Tarekegn F, Seyoum R, Abebe G, Terefe M (2021) Perioperative pediatric mortality in Ethiopia: A prospective cohort study. Ann Med Surg (Lond) 67: 102396.
[Crossref], [Google Scholar], [Indexed]
- Chaibou MS, Daddy H, Dan Mallam MK, Gagara M, James-Didierand L, et al. (2022) Prospective, observational study of perioperative critical incidents, anaesthesia and mortality in elective paediatric surgical patients at a national referral hospital in Niger. South Afr J Anaesth Analg 28: 16-20.
- Montobbio G, Pini-Prato A, Guida E, Disma N, Mameli, et al. (2012) Provisional unicentric experience with an electronic incident reporting form in pediatric anesthesia. Pediatr Anesth 22: 1080-1086.
[Crossref], [Google Scholar], [Indexed]
- Lee JH, Kim EK, Song IK, Kim EH, Kim HS, et al. (2016) Critical incidents, including cardiac arrest, associated with pediatric anesthesia at a tertiary teaching children's hospital. Paediatr Anaesth 26: 409-417.
[Crossref], [Google Scholar], [Indexed]
- Otiobanda GF, Mahoungoun-Guimba KC, Odzebe KWS, Mandavo CM, Boyassa GE, et al. (2011) Pratique de l'anesthésie pédiatrique au centre hospitalier et universitaire de Brazzaville. Rev Afr Anesth Med Urg 16: 3-6.
- Wolfler A, De Silvestri A, Camporesi A, Ivani G, Vittori A, et al. (2020) Pediatric anesthesia practice in Italy: A multicenter national prospective observational study derived from the APRICOT Trial. Minerva Anestesiol 86: 295-303.
[Crossref], [Google Scholar], [Indexed]
- De Graaff JC, Sarfo MC, van Wolfswinkel L, van der Werff DB, Schouten AN, et al. (2015) Anesthesia-related critical incidents in the perioperative period in children; a proposal for an anesthesia-related reporting system for critical incidents in children. Paediatr Anaesth 25: 621-629.
[Crossref], [Google Scholar], [Indexed]
- Zoumenou E, Gbénou S, Assouto P (2010) Pediatric anesthesia in developing countries: Experience in the two main university hospitals of Benin in West Africa. Pediatr Anesth 20: 741-747.
[Crossref], [Google Scholar], [Indexed]
- Abbasi S, Khan FA, Khan S (2018) Pediatric critical incidents reported over 15 years at a tertiary care teaching hospital of a developing country. J Anaesthesiol Clin Pharmacol 34: 78-83.
[Crossref], [Google Scholar], [Indexed]
- Bruder N, Gallula JJ (2007) Evaluation et prise en charge d’un retard de réveil après une anesthésie. Prat Anesth Reanim 11: 122-129.
[Crossref], [Google Scholar]
- Bhaskar SK, Zutshi S, Chanchlani R (2014) Sevoflurane versus halothane for general anesthesia in pediatric patients. A comparative study of induction time, intubation time and emergence time. J Evol Med Dent Sci 3: 2760-2767.
- Shareena T, Ninan R, Kurian MB (2018) Comparative study of induction time and heart rate changes during induction with halothane and sevoflurane in paediatric patients. Int J Contemp Med Res 5:1-6.
[Crossref]
- Soulard A, Babre F, Bordes M, Meymat Y, Sztark F, et al. (2009) Optimal dose of sufentanil in children for intubation after sevoflurane induction without neuromuscular block. Br J Anaesth 102: 680-685.
[Crossref], [Google Scholar], [Indexed]
- Brouh Y, Zoumenou E (2014) Vie professionnelle: Quel regard sur l’anesthésie réanimation en Afrique. Rev Afr Anesth Med Urg 19: 1-2.
- Kurth CD, Tyler D, Heitmiller E, Tosone SR, Martin L, et al. (2014) National pediatric anesthesia safety quality improvement program in the United States. Anesth Analg 119: 112-121.
[Crossref], [Google Scholar], [Indexed]
- Zgleszewski SE, Graham DA, Hickey PR, Brustowicz RM, Odegard KC, et al. (2016) Anesthesiologist- and system-related risk factors for risk-adjusted pediatric anesthesia-related cardiac arrest. Anesth Analg 122: 482-489.
[Crossref], [Google Scholar], [Indexed]
- Christensen RE, Lee AC, Gowen MS, Rettiganti MR, Deshpande JK, et al. (2018) Pediatric perioperative cardiac arrest, death in the off hours: A report from wake up safe, the pediatric quality improvement initiative. Anesth Analg 127: 472-477.
[Crossref], [Google Scholar], [Indexed]
- Wudineh DM, Berhe YW, Chekol WB, Adane H, Workie MM, et al. (2022) Perioperative respiratory adverse events among pediatric surgical patients in University Hospitals in Northwest Ethiopia; A prospective observational study. Front Pediatr 10: 827663.
[Crossref], [Google Scholar], [Indexed]
- N’guessan YF, Coulibaly KT, Abhe CM, Netro D, Mobio MP, et al. (2015) Facteurs pronostics de l’anesthésie pédiatrique en urgence au CHU de Cocody. Anesth Réanim 1: A12.
[Crossref], [Google Scholar]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences