The Effect of Dexmedetomidine on Suppression of the Bispectral Index Score and Hemodynamic Response during Laryngoscopy and Intubation in Addicted Patients in Supratentorial Brain Tumor Surgery
Sara Zandpazandi*, Faranak Behnaz, Davood Ommi and Sogol Asgari
Published Date: 2023-06-30DOI10.35841/2471-982X.9.2.98
Sara Zandpazandi1*, Faranak Behnaz2, Davood Ommi2and Sogol Asgari2
1Department of Neurosurger,Shahid Beheshti University of Medical Sciences, Tehran, Iran
2Department of Anesthesiology, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- *Corresponding Author:
- Sara Zandpazandi
Department of Neurosurgery,
Shahid Beheshti University of Medical Sciences,
Tehran,
Iran,
Email: sarapazandi@gmail.com
Received: February 06, 2023, Manuscript No. IPAPM-23-15814; Editor assigned: February 09, 2023, PreQC No. IPAPM-23-15814 (PQ); Reviewed: February 23, 2023, QC No. IPAPM-23-15814; Revised: June 02, 2023, Manuscript No. IPAPM-23-15814 (R); Published: June 30, 2023, DOI: 10.35841/2471-982X.9.2.98
Citation: Zandpazandi S, Behnaz F, Ommi D, Asgari S (2023) The Effect of Dexmedetomidine on Suppression of the Bispectral Index Score and Hemodynamic Response during Laryngoscopy and Intubation in Addicted Patients in Supratentorial Brain Tumor Surgery. Int J Anesth Pain Med Vol.9 No. 2: 98.
Abstract
Background: Dexmedetomidine is an α2-adrenoceptor agonist that has good sedative effects with no cardiovascular instability or respiratory depression and it might help facilitate endotracheal resection and inhibit hemodynamic responses. This study's objective was to assess how intravenous dexmedetomidine affected cardiovascular response and endotracheal intubation in opium-addict patients.
Materials and methods: This study is a clinically randomized double-blind controlled trial. 100 patient with a diagnosis of supratentorial brain tumor undergoing tumor resection surgery with general anesthesia entered this study. One group received dexmedetomidine (1/μg/kg for 10 minutes) before induction of anesthesia. The same amount of normal saline (placebo) was administered in the second group. The two groups were analyzed statistically regarding BP, HR and BIS, which were recorded before induction of anesthesia, one minute after induction of anesthesia and one minute after intubation. The statistical tests used for analysis are the student T-test, Mann-Whitney non-parametric test, the chi-square test and Fisher's exact test.
Results: Heart rate, Systolic blood pressure and bispectral index scores in the intervention group decreased one minute after anesthesia induction and after intubation compared to the control group. Diastolic blood pressure after induction of anesthesia was not significantly different between the two groups, however, it decreased following the intervention after intubation (p>0.05).
Conclusion: Dexmedetomidine suppressed hemodynamic response and BIS score in opium-addict patients compared to the control group.
Keywords
Dexmedetomidine; Hemodynamic response suppression; Intubation; BIS score
Introduction
Many patients undergoing General Anesthesia (GA) suffer from the stress of following surgery and severe anxiety, which before the induction of anesthesia is at its highest. Sympathetic hyperactivity due to this type of anxiety is exacerbated by laryngoscopic manipulation, endotracheal intubation and surgical stimulation stimulating the sympathetic nervous system and increasing catecholamine secretion, eventually increasing Heart Rate (HR), vascular resistance and decreased cardiac output. This response begins immediately after intubation, lasts 5 to 10 minutes and can lead to severe situations such as myocardial ischemia, arrhythmias and cerebrovascular accidents for patients at risk of hypertension and ischemic heart disease. To deliver sedation and preserve hemodynamic stability before and after intubation, one of the main objectives of anesthetic management is to reduce body temperature [1].
Opioids, beta-blockers and local anesthetics to avoid alterations in the cardiovascular system are used when performing endotracheal intubation. Drug addiction is an essential factor that should be seriously considered in the field of anesthesia, as addicted patients may need higher doses of anesthetics compared to non-addicted people and hemodynamic changes following laryngoscopy may also be more severe in addicted patients. On the other hand, the overuse of anesthetics results in hemodynamic instability and protracted recovery, which is difficult for anesthesiologists. Short-acting opioids such as remifentanil have been reported to be useful in stabilizing patients conditions, intraoperative hemodynamics and rapid recovery in patients.
However, these drugs cause numerous postoperative problems, such as acute opioid tolerance and postoperative pain. Dexmedetomidine (DEX), i.e., a selective α2 agonist was introduced in 1999 for human use. Dexmedetomidine has an 8 times higher affinity to α2-adrenoceptors than clonidine with all the characteristics of an α2 agonist with preferably no respiratory depression side effects. Dexmedetomidine is an imidazoline derivative that selectively acts as an agonist on alpha-2 receptors and inhibits the release and uptake of norepinephrine by reducing sympathetic activity. This α2 agonist acts through three types of α2-α2A, α2B and α2C receptors located in the spinal cord and other organs.
Stimulation of 2A and 2C receptors in the locus coeruleus leads to sedation. Activation of both 2A and 2C receptors directly inhibits pain transmission by decreasing the release of substance P in the spinal cord. Agonism at the α-2B receptor in the hypothalamic thermoregulatory center of the brain suppresses shivering, causes pain in the spinal cord and causes arteries to constrict in the peripheral arteries. It increases the sensitivity of cardiac baroreceptors and also reduces the stress response to surgical stimuli. These conditions may help reduce the dose of narcotics and anesthesia, as well as the need for postoperative analgesia. Since, DEX prevents empathetic input, the sympathetic reaction to intubation and surgery is weakened as a result. According to previous reports, its analgesic impact can cut the requirement for postoperative opioids by 30 to 50 percent. Dexmedetomidine also provides sedation without respiratory depression which is currently routinely utilized as a sedative in surgery or intensive care. In terms of analgesia and patient and physician satisfaction, DEX has reportedly outperformed other sedatives, such as midazolam, without resulting in additional cardiac problems.
In neuroesthesia, such as elective surgery for a supratentorial brain tumor, appropriate surgical conditions make the brain less affected by the procedure and less likely to self-regulate cerebral circulation. Prevention of hypertensive responses during the recovery phase has been reported to be an important issue in reducing intracranial hemorrhage in these procedures. Another important consideration is the duration of action of medications that are used to stop breathing following extubation. When repeated dosages of fentanyl are administered, one of its drawbacks is a long-term respiratory compromise. This study is conducted to determine how dexmedetomidine affects hemodynamic response suppression and endotracheal intubation in opioid-addicted patients undergoing surgical resection of supratentorial brain tumors.
Materials and Methods
The study was conducted by the declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of Shahid Beheshti medical university, code: MSP.REC.1398.126 and approved by the Iranian Registry of Clinical Trial (IRCT), IRCT code: 2020112204946N1. Also, an individual, written and signed informed consent for this RCT analysis was obtained from each participant. This study is a clinically randomized double-blinded controlled trial. Patients with a diagnosis of supratentorial brain tumor undergoing tumor resection surgery entered this study [2].
The inclusion criteria were:
• Age 18-65 years.
• Consumption of at least 4 grams of natural opium or synthetic alkaloids each day either orally or inhaled for over six months.
• Class I and II physical conditions (ASA score).
• Duration of operation of lower than 4 hours; systolic blood pressure between 90 mm Hg-140 mm Hg in the 24 hours before surgery; SPO2 of more than 90% without oxygen therapy and normal body temperature between 36.8 and 37.2 degrees celsius.
All participants underwent general and systemic physical examinations before anesthesia. All patients took standard lab tests, such as a Complete Blood Count (CBC), Liver Function Tests (LFT), Renal Function Tests (RFT), Electrocardiography (ECG) and Chest X-ray (CXR). Patients were NPO (nothing by mouth) for eight hours before the surgery [3].
The exclusion criteria were:
• Patients for whom a difficult airway for intubation was predicted by the anesthesiologist.
• Laryngoscopy time more than 20 seconds (from the time of laryngoscope blade entrance until complete intubation).
• A history of high blood pressure, diabetes, liver disease or kidney disease.
• Taking beta-blockers and any type of medication related to blood pressure in the 24 hours before surgery.
• Patients who have a history of gastrointestinal disease, multiple fractures or trauma, coronary artery disease or arrhythmia.
• Pregnant or lactating women.
Sample size calculation and randomization
The 80% power, 5% error, the effect size of about 40%, or the risk ratio of about 3% in the two groups and the 1:1 ratio in the two groups were all measured using the following formula:
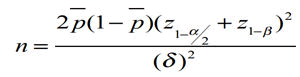
At least 50 patients in each group should be entered, considering a 5% drop in the total amount obtained from the computations.
With computer-based software, we used a 1:1 aspect ratio to randomly assign patients to two groups of case, to receive dexmedetomidine or control, to receive a placebo. Either case or control group consisted of 50 patients. Computer-generated random numbers were used for randomization. This was carried out by an anesthesiologist who was not involved in medication prescription or outcome monitoring and was not aware of the study methodology through a calculator online at www.calculation.net and using the results of the calculator, numbers from 1 to 50 were assigned to the control group and those in the intervention group were numbers from 51 to 100. In addition, both groups were not significant in terms of age and sex frequency distribution. Blinding the patients into the intervention or control groups and the results and information were recorded by a person who did not know about the groups [4].
Each patient was given a sealed envelope containing case or control group information and returned by the designated nurse in the operating room. Patients were blinded in the matter of group designation and interventions (DEX or placebo). However the anesthesiologist in the operating room was aware of the type of medication to administer. One senior anesthesiologist (senior author) prepared and prescribed all administered drugs. Patients, healthcare staff, statisticians and research group members were also blinded to case and control groups.
Each patient received premedication with fentanyl 3 g/kg -5 g/kg and midazolam 0.03 mg/kg. Two groups of 50 patients were formed by randomly dividing the patients. 10 minutes before induction of anesthesia, the case group received dexmedetomidine (1 μg/kg) infused intravenously while the control group received an equivalent amount of 0.09% NS. Then, all participants received induction of anesthesia atracurium 0.5 mg/kg, and propofol 1 mg/kg to 2.5 mg/kg, which lasted three minutes. In addition to standard monitoring, deep anesthesia monitoring, Bispectral index (BIS) and neuromuscular monitoring were performed for every patient. After the neuromuscular response vanished, based on neuromuscular monitoring, patients underwent direct laryngoscopy with an appropriate tube size. The location of the inserted tube was confirmed by both hearing and capnography. BP, HR and BIS were recorded before induction of anesthesia, one minute after induction of anesthesia and one minute after intubation.
Variables were expressed as means and standard deviations and qualitative variables as numbers (percentages). If necessary, the Mann-Whitney non-parametric test and the student T-test were used to compare the quantitative variables between the two groups. The qualitative characteristics of the two groups were compared using the chi-square and Fisher's exact tests. To compare the variables that were measured over time (longitudinal data), the value of the repeated measures analysis of variance (repeated measure ANOVA) was used and the value of the variable was entered into the model as a covariate and the effect of this variable was corrected. Statistical test was performed in two domains with a significance level of 5% (P value=0.05). SPSS 26 software was used for data analysis [5].
Results
Regarding age, gender, height, weight and ASA physical condition score, there were no statistically significant differences between the groups (P<0.05). The mean age was 41.88 ± 14.64 in the intervention group compared to 41.70 ± 13.22 in the control group (P=0.494). Also, the mean weight of patients in the intervention group was 71.02 ± 13.19 and in the control group was 69.32 ± 11.33. The mean GCS in the intervention group was 15.00 ± 0.0 and in the control group was 15.00 ± 0.0 which was not significantly different (P>=0.999).
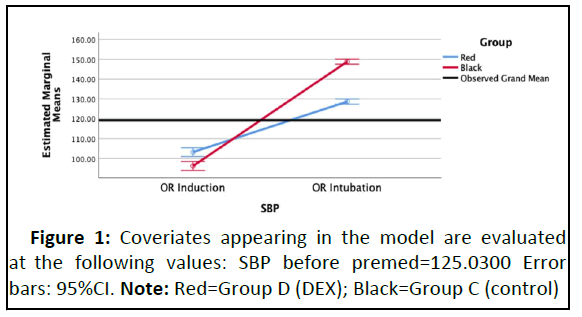
Mean systolic blood pressure before the drug administration was not significantly different between the case and control groups (P=0.738). One minute after induction of anesthesia, the mean systolic blood pressure in the intervention group was 103.24 ± 8.97 and in the control group was 96.08 ± 7.05, which were significantly different (P<0.001). Also, the mean systolic blood pressure one minute after intubation was 128.64 ± 3.86 in the intervention group and 148.78 ± 5.30 in the control group, which were significantly different (P<0.001) [6].
Table 1 displays the blood pressure of patients. The difference in systolic blood pressure on intervals of anesthesia induction and intubation is significant. Also, in general, the trend of systolic blood pressure (the effect of baseline time is corrected) between the two groups is significantly different, which can be seen in the relevant chart (Figure 1).
| SBP | D n=50 | C n=50 | P-value |
|---|---|---|---|
| Before premed | 125.64 ± 8.81 | 124.42 ± 17.79 | 0.738 |
| Anestheia induction | 103.24 ± 8.97 | 96.08 ± 7.05 | <0.001 |
| Intubation | 128.64 ± 3.86 | 148.78 ± 5.30 | <0.001 |
| Total* | - | - | <0.001 |
Note: *Repeated measures ANOVA; using SBP before Premed as the covariate
Table 1: Patients systolic blood pressure between induction anesthesia and intubation.
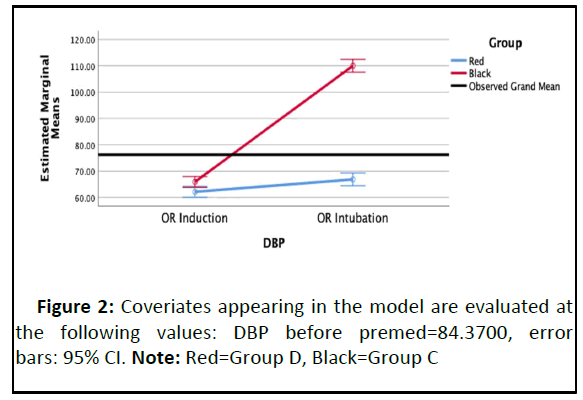
The mean diastolic blood pressure before drug administration was not significantly different between the intervention and control groups (P=0.779). One minute after induction of anesthesia, the mean diastolic blood pressure in the intervention group was 62.14 ± 7.45 and in the control group was 65.90 ± 7.10, which was not significantly different (P=0.011), but the mean diastolic blood pressure one minute after intubation in the intervention group was 66.48 ± 9.96 and in the control group 110.00 ± 7.04 which had a significant difference (P<0.001) (Table 2 and Figure 2) [7].
| DBP | D n=50 | C n=50 | P-value |
|---|---|---|---|
| Before premed | 84.28 ± 5.04 | 84.46 ± 4.21 | 0.779 |
| OR induction | 62.14 ± 7.45 | 65.90 ± 7.10 | 0.011 |
| OR intubation | 66.84 ± 9.96 | 110.00 ± 7.04 | <0.001 |
| Total* | - | - | <0.001 |
Note: *Repeated measures anova; using DBP before Premed as the covariate
Table 2: The mean diastolic blood pressure before drug administration.
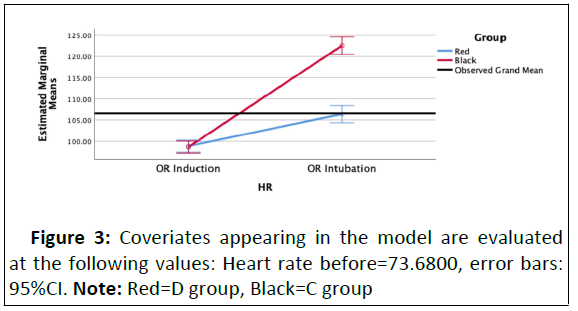
The mean heart rate before drug administration and after induction of anesthesia was not significantly different between the intervention and control groups, but one minute after intubation, the mean heart rate in the control group was significantly higher than the intervention group (P<0.001) (Table 3 and Figure 3).
| DBP | D n=50 | C n=50 | P-value |
|---|---|---|---|
| Heart rate | |||
| Before Premed | 73.92 ± 8.00 | 73.44 ± 6.35 | 0.774 |
| OR Induction | 99.00 ± 7.07 | 98.52 ± 5.23 | 0.722 |
| OR Intubation | 106.52 ± 8.75 | 122.38 ± 0.33 | <0.001 |
| Total* | - | - | <0.001 |
Table 3: Mean heart rate before drug administration and after induction of anesthesia.
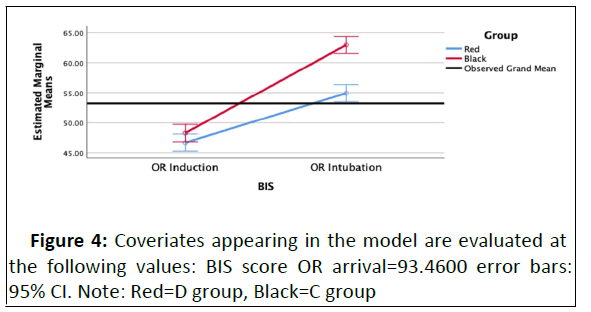
This indicates that hemodynamic changes during intubation are less in opium-addicted patients who received dexmedetomidine before induction of anesthesia. In terms of changes in anesthesia depth (BIS), patients in the intervention group one minute after intubation had a lower mean BIS score than the control group, which was a significant difference (P<0.001). The mean BIS score in the intervention group one minute after intubation was 54.84 ± 3.16 and in the control group was 63.04 ± 5.65 (Table 4 and Figure 4) [8].
| BIS score | D n=50 | N c=50 | P-value |
|---|---|---|---|
| Before premed | 96.64 ± 0.85 | 90.28 ± 6.90 | <0.001 |
| OR induction | 46.24 ± 3.84 | 48.78 ± 5.44 | 0.023 |
| OR intubation | 54.84 ± 3.16 | 63.04 ± 5.65 | <0.001 |
| Total* | - | - | <0.001 |
Note: *Repeated measures ANOVA; using BIS Before Premed as the covariate
Table 4: The mean BIS score in the intervention group one minute after intubation.
Discussion
Anesthesia and surgical procedure are associated with increased stress, which manifests as tachycardia, hypertension and increased sympathetic activity. Laryngoscopy and intubation are stressful stimuli that increase blood catecholamine levels, cause tachycardia and hypertension and are more common in opium abusers. Numerous techniques, including inhalation anesthetics, lidocaine, opioids, calcium channel blockers, and direct-acting vasodilators, have been utilized to lower these reactions. Dexmedetomidine, a strong alpha-2 agonist, has recently been demonstrated to have the potential to lower the stress response, respiratory depression, bradycardia, hypotension, sedation and other adverse effects. The current study's objective was to assess how dexmedetomidine affects opiate abusers hemodynamic responses to laryngoscopy and endotracheal intubation [9].
Before drug injection and upon entering the operating room, all patients demographics, blood pressure, heart rate and GCS were measured which were not significantly different between the two groups. One minute after anesthesia induction and after laryngoscopy and intubation, this difference was statistically significant between the two groups. Patients in the intervention group had lower BIS scores and fewer hemodynamic changes after anesthesia induction and after intubation [10].
In 2018 Sandeep reported how esmolol and dexmedetomidine affect adult patients who underwent elective surgery’s laryngoscopy and intubation in terms of suppressing the hemodynamic response. Dexmedetomidine and esmolol both decreased the hemodynamic response to intubation compared to the control group, furthermore, DEX maintained hemodynamic stability.
Dexmedetomidine's impact on hemodynamic responses during laryngoscopy and intubation in laparoscopic surgery was studied by in 2018. In this study, two groups of 30 patients each were randomly assigned from a total of 60 patients of both sexes between the ages of 18 and 65 who underwent elective laparoscopic procedures. Before induction for more than 10 minutes, Group DEX received a loading dose of 1 g/kg of injectable DEX and then a 0.2 g/kg/hour maintenance dosage. The same dose of normal saline was given to group salin as the control group. They noticed that after intubation and throughout the pneumoperitoneum period, heart rate, systolic blood pressure, diastolic blood pressure and mean arterial pressure were significantly lower. They ultimately concluded that DEX decreases the hemodynamic response to intubation, laryngoscopy and pneumoperitoneum [11].
A comparison of the effectiveness of fentanyl and dexmedetomidine in lowering the reaction to laryngoscopy and intubation was reported by Rani et al. and Gunalan et al. DEX was superior to fentanyl in regulating HR and Mean Arterial Pressure (MAP) during laryngoscopy and intubation, according to Gunalan et al. DEX and fentanyl both decrease laryngoscopic and intubation responses, according to Mahjoubifard's investigation on the effects of DEX, lidocaine and fentanyl on hemodynamic responses to intubation in 2020. However, the DEX group had higher levels of bradycardia and hypotension. Tanskanen et al. used DEX in patients undergoing intracranial tumor surgery. They demonstrated that DEX lowered tachycardia and hypertensive response during intubation and extubation more effectively than placebo.
According to the authors of the same study, DEX decreased SAP by 20% intraoperatively compared to control levels. Dexmedetomidine provided during neuro-esthesia decreases the need for opioids, results in lower antihypertensive treatments and improves hemodynamic stability during incision. In another study, Ilhan et al. Fentanyl and DEX's effects on supratentorial craniotomy adjuvants were examined. It regulates the postoperative period and is safer and more effective than the conventional drugs used in managing hemodynamic changes during surgical stimulation [12].
Batra et al., also reported in 2017 that initiating preintracranial DEX infusion maintained hemodynamic stability during surgery and was effective in reducing cardiovascular responses to intubation, the use of cranial pins, extubation and the need for other anesthetics [13].
Mirkhashti et al., investigated the effect of topical DEX on the sedative dose during endotracheal intubation. This study showed that the use of topical DEX can reduce the needing dosage of anesthetics during the procedure. Topical DEX has no systemic side effects such as decreased arterial oxygen saturation or decreased heart rate. Also in a study in 2019, Masoudifar et al. compared the effect of midazolam and dexmedetomidine on the sedation level, hemodynamics and complications in stereotaxic surgery. They concluded that DEX is preferred over midazolam in sensitive surgeries since it has predominance in hemodynamic stability and causes fewer respiratory complications than midazolam [14].
Jafari et al., presented that intravenous administration of dexmedetomidine and magnesium sulfate in patients with drug abuse under spinal anesthesia reduced the need for intraoperative opioids and delayed the first time of drug recovery and significantly reduced the mean Verbal Numerical Rating Score (VNRS), which was measured over time, compared to the control group. In the study by in 2019, which investigated the effects of dexmedetomidine on hemodynamic responses during endotracheal resection and the amount of sedation in recovery following cholecystectomy, was shown that intravenous infusion of DEX at a dose of 0.8 μg/kg, 10 minutes before endotracheal tube removal, stabilizes patients hemodynamics and facilitates extubation [15].
Conclusion
Finally, the results of our study suggest that preoperative administration of dexmedetomidine in major surgeries such as supratentorial tumor resection in opioid-addicted patients can suppress hemodynamic responses during laryngoscopy and intubation. Furthermore, these patients also have lower BIS scores.
Acknowledgment
The authors express their sincere thanks to the staff of Shohada Tajrish hospital, Shahid Beheshti university of medical sciences, Tehran, Iran, for their assistance.
Funding
This research received no specific grant or funding from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of Interest
The authors declare no conflict of interest to declare. The authors certify that they and their family members have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers bureaus; membership, employment, consultancies, stock ownership or other equity interest and expert testimony or patent-licensing arrangements) or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript. The authors have no conflict of interest to declare.
References
- Kim JW, Lee HL, Park JS, Kim JH, Ryu KH, et al. (2018) Pre-anesthetic sedative effect of dexmedetomidine in laparoscopic cholecystectomy performed under general anesthesia. Anesth Pain Med 13: 23-29.
- Roy WL, Edelist G, Gilbert B (1979) Myocardial ischemia during non-cardiac surgical procedures in patients with coronary-artery disease. Anesthesiol 51: 393-397.
- Siedlecki J (1975) Disturbances in the function of cardiovascular system in patients following endotracheal intubation and attempts of their prevention by pharmacological bloackade of sympathetic system. Anaest Res Int Therap 3: 107-123.
- Stanley TH, Berman L, Green O, Robertson D (1980) Plasma catecholamine and cortisol responses to fentanyl-oxygen anesthesia for coronary-artery operations. J Amer Soc Anesthesiol 53: 250-253.
[Crossref] [Google Scholar] [PubMed]
- Stoelting RK (1978) Blood pressure and heart rate changes during short-duration laryngoscopy for tracheal intubation: Influence of viscous or intravenous lidocaine. Anest Analg 57: 197-199.
[Crossref] [Google Scholar] [PubMed]
- Farsani DM, Ghadimi K, Abrishamkar R, Montazeri K, Peyman A, et al. (2021) Evaluating sedative effects of dexmedetomidine and morphine in the patients with opioid use disorder undergoing cataract surgery. Ame J Clin Exp Immunol 10: 30.
[Google Scholar] [PubMed]
- Ciftci T, Erbatur S, Ak M (2015) Comparison of the effects of dexmedetomidine and remifentanil on potential extreme haemodynamic and respiratory response following mask ventilation and laryngoscopy in patients with mandibular fractures. Eur Rev Med Pharmacol Sci 19: 4427-4433.
[Google Scholar] [PubMed]
- Verma AK, Verma S, Barik AK, Kanaujia V, Arya S, et al. (2021) Intubating conditions and hemodynamic changes during awake fiberoptic intubation using fentanyl with ketamine versus dexmedetomidine for anticipated difficult airway: A randomized clinical trial. Braz J Anesthesiol 71: 259-264.
[Crossref] [Google Scholar] [PubMed]
- Aouad MT, Zeeni C, Al Nawwar R, Siddik-Sayyid SM, Barakat HB, et al. (2019) Dexmedetomidine for improved quality of emergence from general anesthesia: A dose-finding study. Anest Ana 129: 1504-1511.
[Crossref] [Google Scholar] [PubMed]
- Basali A, Mascha EJ, Kalfas I, Schubert A (2000) Relation between perioperative hypertension and intracranial hemorrhage after craniotomy. J Amer Soc Anesthesiol 93: 48-54.
[Crossref] [Google Scholar] [PubMed]
- Guy J, Hindman BJ, Baker KZ, Borel CO, Maktabi M, et al. (1997) Comparison of remifentanil and fentanyl in patients undergoing craniotomy for supratentorial space-occupying lesions. J Amer Soc Anesthesiol 86: 514-524.
[Crossref] [Google Scholar] [PubMed]
- Sharma S, Suthar OP, Tak M, Thanvi A, Paliwal N, et al. (2018) Comparison of esmolol and dexmedetomidine for suppression of hemodynamic response to laryngoscopy and endotracheal intubation in adult patients undergoing elective general surgery: A prospective, randomized controlled double- blinded study. Anest Essay Res 12: 262.
[Crossref] [Google Scholar] [PubMed]
- Gupta S, Agarwal S, Jethava D, Choudhary B (2018) Effect of dexmedetomidine on hemodynamic changes during laryngoscopy, intubation and perioperatively in laparoscopic surgeries. Ind J Healt Sci Biomed Res 11: 265.
- Rani P, Kumar VH, Ravishankar M, Sivashanmugam T, Sripriya R, et al. Rapid and reliable smooth extubation comparison of fentanyl with dexmedetomidine: A randomized, double-blind clinical trial. Anest Essay Res 10: 597.
[Crossref] [Google Scholar] [PubMed]
- Gunalan S, Venkatraman R, Sivarajan G, Sunder P (2015) Comparative evaluation of bolus administration of dexmedetomidine and fentanyl for stress attenuation during laryngoscopy and endotracheal intubation. J Clin Diagn Res 9: UC06.
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences