Case Report: Peripheral Nerve Block in a Pregnant Patient
Deniz Turan * , Fatma Gülçin Öztürk Arikan, Serdar Epözdemir and Sezai Ozkan
DOI10.36648/2471-982X.21.7.38
Deniz Turan*, Fatma Gülçin Öztürk Arikan, Serdar Epözdemir and Sezai Ozkan
Istanbul Medipol University Camlica Hospital, Anesthesia and Reanimation Clinic, Istanbul, Turkey
- *Corresponding Author:
- Deniz Turan
Istanbul Medipol University Camlica Hospital
Anesthesia and Reanimation Clinic
Istanbul
Turkey
Tel: 533 025 1909
E-mail: denizturan@medipol.edu.tr
Received Date: March 12, 2021; Accepted Date: March 26, 2021; Published Date: April 02, 2021
Citation: Turan D, Arikan OGF, Epözdemir S, Ozkan S (2021) Case Report: Peripheral Nerve Block in a Pregnant Patient. Int J Anesth Pain Med Vol.7 No.3:38
Abstract
In general, peripheral regional blocks are applied less frequently than central blocks. There are few publications about regional blocks applied in the upper extremity of pregnant women. In this case report, we aimed to share the peripheral nerve block application we applied to our 20 weeks old pregnant patient who was scheduled for surgery due to stab injury in the left hand thenar region. During the operation, the patient did not need any analgesics or sedatives. No complications were encountered during the operation. No analgesic was required for 8-10 hours in the postoperative period. The patient, who was controlled by the obstetrics clinic in the postoperative period, was evaluated as normal. The patient was discharged on the second day after the controls. In conclusion, we consider peripheral nerve blocks as the anesthesia method that should be preferred over general anesthesia in eligible pregnant patients undergoing non-obstetric intervention.
Keywords
Algology; Obstetric anesthesia; Orthopedic anesthesia; Peripheral nerve block; Dynamic congruency
Introduction
During pregnancy, the rate of need for surgery for reasons other than pregnancy has been reported to be 0.3%-2.2%. It has been reported that 42% of these operations were performed in the first 3 months of pregnancy (1st trimester), 35% in the 2nd trimester (2nd trimester) of pregnancy, and 23% in the last trimester [1]. Operation and anesthesia during pregnancy are very important in terms of complications that may develop for both mother and baby [2].
It may be encountered during general anesthesia in pregnant patients; Regional anesthesia is prioritized due to difficulty in airway control, hypoxemia, aspiration risk and also the negative effects of anesthetic agents on the mother and fetus [3,4].
In general, peripheral regional blocks are applied less frequently than central blocks: There are few publications about regional blocks applied in the upper extremity in pregnant women. In this case report, we aimed to share the peripheral nerve block application we applied to our 20 weeks old pregnant patient who was scheduled for surgery due to stab injury in the left hand thenar region.
Case Presentation
A 31-year-old, 75 kg, 20-week-old pregnant patient with a Body Mass Index (BMI) of 27 kg m2, applied to the emergency department when the knife stuck in the left hand thenar area while working in the kitchen came out of the back of the hand. In the examination of the patient performed by an orthopedic physician, a total sensation defect in the radial face of the 2nd finger was observed, and surgical exploration was planned for the patient. In the patient's story before the accident; no neurological deficit, local anesthetic allergy, coagulopathy, and skin infection at the block site were confirmed.
Due to the anatomical location of the area where the operation was planned, it was decided to perform only median and radial nerve block. Preoperative and postoperative sedative drugs were not administered to the patient, who received informed consent for surgery and anesthesia. The patient's Arterial Blood Pressure (ABP), Peak Heart Rate (HR) and Peripheral Oxygen Saturation (SpO2) were monitored.
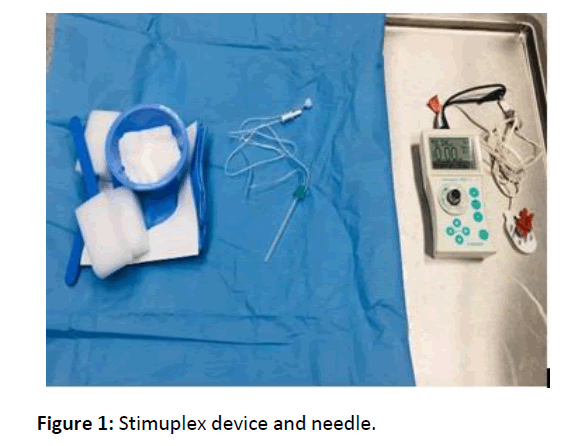
To apply the block, a peripheral nerve stimulator (Stimuplex® HNS 11-Braun, Germany) and a plexus needle Stimupleks A® (B. Braun Melsungen AG, Japan) 21G, 50 mm were used. The cathode pole of the nerve stimulator was connected to the conductive end of the needle and the anode pole to the ECG electrode attached to the deltoid muscle. With the stimulator, initially with the help of a 2 mA current, the skin was entered with a needle in an anteroposterior manner, by forming a right angle to the floor where the patient was lying, from the intervention point marked in the axillary region.
The motor responses of the muscles innervated by the nervus medianus and nervus radialis were searched according to their twitching movements. Twitching was also observed at 0.4 mA, and after the aspiration test, the patient had twitching movements of the nervus medianus and nervus radialis, and after the aspiration test, a total of 20 (10 ml 0.5% bupivacaine, 5 ml 2% lidocaine and 5 ml saline) 1 ml of solution was given. In total, 40 ml of solution was given.
After the application, at the 5th, 10th, 15th, 20th and 30th minutes, the musculocutaneous, radial, median and ulnar nerve traces were evaluated by the sensory block level (pin-prick) method (0=no block, 1=sense of touch, no pain, 2=sense of touch and no pain), and motor block levels were evaluated using the Bromage scale (0=no block, 1=moderate loss of motion, 2=complete motor block). The places where there was no sense of touch were evaluated as anesthetized and the operation was started in the 30th minute (Figure 1).
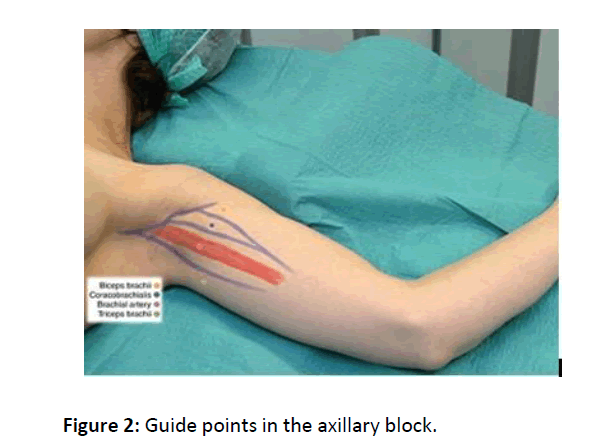
The operation of the patient took 72 minutes. During the operation, the patient did not need any analgesics or sedatives. No complications were encountered during the operation. There was no need for analgesic for 8-10 hours in the postoperative period. The patient, who was controlled by the gynaecology clinic in the postoperative period, was evaluated as normal. The patient was discharged on the second day after the controls (Figure 2).
Results and Discussion
Sensitivity to anesthetics increases during pregnancy [5]. Although it is not a proven agent among anesthetic agents to affect premature labor, it should be kept in mind that every operation performed may cause premature labor. Considering all these conditions, regional anesthesia seems more advantageous than general anesthesia in eligible patients. Although undesirable effects such as nausea and vomiting are observed less frequently after peripheral regional block; there is a small risk of intraneural injection, hematoma and intravasal injection [6].
With the widespread use of ultrasonography (USG) in recent years, it has led to a change in block preferences in clinical practice. Due to the risk of pneumothorax, supraclavicular and infraclavicular blocks, which are applied less frequently with blind techniques, have started to be applied more widely because USG provides visual guidance [7,8].
Many reasons can affect the success of the block, especially the experience of the practitioner and the technique used. A homogeneous success rate has been achieved by using USG in regional anesthesia. Over time, the techniques have become more refined, the block indications are more clearly defined, the possible physiological effects are better understood, and the complications are better known. Visual guidance obtained with USG and increasing success rates increased the interest in regional anesthesia [9].
Since USG is not available in our clinic, axillary block is a common anesthesia practice we use in forearm surgeries because of its easy application in peripheral nerve blocks and its low risk of complications. However, patient comfort is adversely affected during application due to the need for multiple injections. Decreasing the amount of injection will provide comfort for both the patient and the practicing clinician. Reducing the number of injections from 3 to 2 both reduces the time and increases patient comfort [10,11].
The axillary block applied with the double injection method provides sufficient sensory and motor block as much as the multiple injection method. In addition, there is less need for additional injection than the single injection method [12].
In our case, the axillary block method applied with 2 injections was successfully performed. Sufficient sensory and motor block was provided and additional injection was not needed. In addition, the case that did not need analgesic for 10 hours in the postoperative period was successfully managed using a minimum of systemic drugs. No pathology was found in the fetus in the patient who had postoperative perinatology control. The patient, who was delivered by cesarean section under spinal anesthesia at her 39th week, gave birth to a healthy baby.
Conclusion
In conclusion, we consider peripheral nerve blocks as the anesthesia method that should be preferred over general anesthesia in eligible pregnant patients undergoing non- obstetric intervention.
References
- Reitman E, Flood P (2011) Anesthetic considerations for non-obstetric surgery during pregnancy. Br J Anaesth 107: 72-78
- Günaydin B (2012) Anesthesia management in surgical interventions not related to pregnancy. Turkish Anest Rean Der Journal 40: 1-10.
- Divatia JV, Bhowmick K (2005) Complications of endotracheal intubation and other airway management procedures. Indian J Anaesth 49: 308-318.
- Frerk C, Mitchell VS, McNarry AF, Mendonca K, Bhagrath R, et al. (2015) Difficult Airway Society intubation guidelines working group. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. British J Anaesth 115: 827-848
- Hakimoglu S, Karcioglu M, Tuzcu K, Koyuncu O, Turhanoglu S (2015) Anesthetic approach to a pregnant patient with forearm flexor tendon injury. Mustafa Kemal Univ Medical Journal 6: 65-68.
- Kizliay D, Ayten Saraçoglu A, Bezen O, Kafali IH (2017) Midhumeral block application for non-obstetric surgical intervention during pregnancy. J Anesth 25: 101-104.
- Perlas A, Lobo G, Lo N, Brull R, Chan VW, et al. (2009) Ultrasound-guided supraclavicular block: Outcome of 510 consecutive cases. Reg Anesth Pain Med 34: 171-176.
- Gurkan Y, Hosten T, Tekin M, Acar S, Solak M, et al. (2012) Comparison of ultrasound-guided supraclavicular and infraclavicular approaches for brachial plexus blockade. Agri 159-164
- Koscielniak-Nielsen ZJ (2008) Ultrasound-guided peripheral nerve blocks: What are the benefits? Acta Anaesthesiol Scand 52: 727-737
- Yonca Y, Mehtap O, Nurten B (2014) Our experiences with a single injection axillary block technique. North Clin Istanb 1: 39-44.
- Sia S, Lepri A, Ponzecchi P (2001) Axillary brachial plexus block using peripheral nerve stimulator: A comparison between double and triple-injection techniques. Reg Anesth Pain Med 26: 499-503
- Inberg P, Annila I, Annila (1999) Double-injection method using peripheral nerve stimulator is superior to single injection in axillary plexus block. Reg Anesth Pain Med 24: 509-513
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences