Bar Code-Assisted Medication Labeling: A Novel System to Improve Efficiency and Patient Safety
Karen C. Nanji, Kyle A. Vernest, Nathaniel M. Sims, William D. Driscoll Wilton C Levine
Karen C. Nanji, Kyle A. Vernest, Nathaniel M. Sims, William D. Driscoll Wilton C Levine*
Massachusetts General Hospital, Boston, MA, USA
- Corresponding Author:
- Wilton C. Levine
Department of Anesthesia
Critical Care and Pain Medicine
Massachusetts General Hospital
55 Fruit Streetm, Boston MA, 02114
Tel: 617-726-3891
E-mail: wlevine@partners.org
Abstract
Background: Medication errors in anesthesia present patient safety challenges and research has shown that proper medication labeling may reduce error rates. Bar code-assisted syringe labeling may improve labeling accuracy and compliance. The purpose of this study is to compare the time required to label syringes using the manual method with the time required using bar code-assisted syringe labeling technology; to determine labeling error rates and compliance with Joint Commission (JC)-required labeling data elements; and to determine user satisfaction with the syringe labeling technology.
Methods: We observed clinicians during preparation of three medications (Succinylcholine, Propofol and Atropine) using the conventional manual labeling technique and a bar code-assisted syringe labeling system. Participants completed a survey about their experiences using the bar codeassisted medication labeling system. Primary outcome measures were time to prepare medications, JC labeling compliance and labeling errors.
Results: Sixty-four subjects prepared 192 syringes using each method. Total time to prepare the drugs was shorter using the bar code-assisted system (129.9s vs. 138.6s, p=0.01). With the manual labeling method, we observed 38 errors on 24 labels (12.5% label error rate). No errors were found using the bar code-assisted syringe labeling system. Furthermore, survey data revealed >95% clinician satisfaction with the system.
Conclusions: More than one in ten manually labeled syringes contained errors. Bar code-assisted medication labeling not only ensured 100% accuracy and compliance with JC labeling requirements but was also faster than the conventional manual method, even for first time users with no training. Bar code technology has the potential to save time while improving perioperative patient safety.
Introduction
Medication administration in anesthesia presents patient safety challenges. Syringe swaps, ampoule swaps, and wrong dose errors can cause serious harm [1]. In fact, the most frequently cited critical incidents in anesthesia are drug administration errors [2]. The literature on anesthesia medication error rates is sparse. In one study, the reported anesthesia drug administration error rate was one per 133 anesthetics [3]. In another study, 85% of anesthesiologists reported at least one drug error or near miss during their careers [4].
The literature shows that that proper syringe labeling can reduce medication error rates [1,5]. In addition, 84% of anesthesiologists agreed that improved standards for drug labeling would reduce the incidence of medication errors [4]. Despite knowing that improved labeling practice can help decrease drug administration errors, anesthesiologists struggle to fully label drugs in the perioperative environment [5].
Due to the independent nature of anesthesia practice, clinicians do not routinely have help to perform redundant checks on every drug label and drug administration. The addition of another clinician to each operating room to perform a second check would be cost prohibitive for most anesthesia practices and hospitals. Nonetheless, anesthesiologists need a system to allow such double-checking and other safety checks at the time of drug preparation and drug administration.
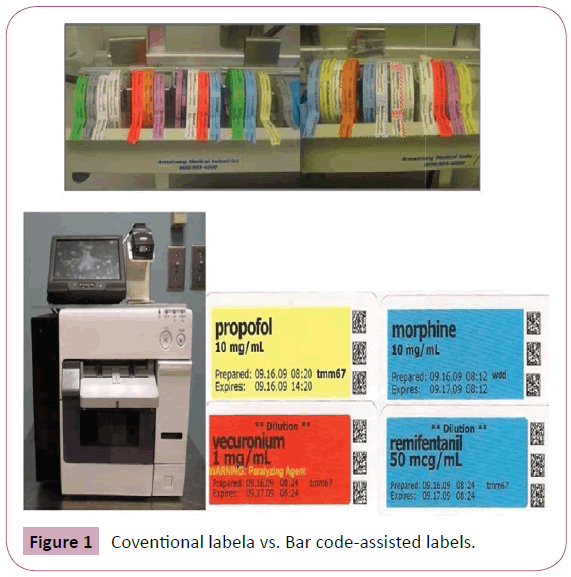
To meet this need, our institution developed a bar code-assisted syringe labeling technology that scans the FDA-mandated, manufacturer-issued barcode on each medication vial, and prints a waterproof color label (Figure 1) containing the 2011 Joint Commission (JC) National Patient Safety Goal required labeling data elements, which include, at a minimum: drug name, strength, quantity, diluent and diluent volume (if not apparent from container), expiration date and time when not used within 24 hr [6-8]. The system also provides safety features including audio and visual readback of drug name and concentration as well as clinical alerts for recalled and expired vials. The label can be easily integrated with anesthesia information management systems (AIMS), via a two-dimensional barcode printed on each label, to enhance their value with clinical alerts such as drugdrug interactions at time of administration. The integration of bar code-assisted syringe labels with AIMS may facilitate real-time clinical documentation.
The purpose of this study is to compare the time required to label syringes using the manual method with the time required using the bar code-assisted syringe labeling technology; to determine the labeling error rates and compliance with JC labeling requirements; and to determine user satisfaction with the syringe labeling technology at a large academic teaching hospital.
Materials and Methods
After obtaining institutional review board approval, we contacted by E-mail all anesthesia clinicians at our center, including staff anesthesiologists, anesthesia residents and Certified Registered Nurse Anesthetists (CRNAs), to invite them to participate in our study. We set up an anesthesia workstation with a drug tray and workspace at the operating room pharmacy. Interested clinicians came to the workstation, over a two week period in 2009, to participate in the study. There were no exclusion criteria. Verbal consent was obtained from all participants, and participants were able to withdraw from the study at any time.
We observed and timed anesthesia clinicians during preparation of three medications (Succinylcholine, Propofol and Atropine) using both the conventional manual technique and the bar codeassisted syringe labeling system. The time taken to prepare the medications using each method was recorded. Labeling errors and compliance with the labeling requirements were assessed for each method. Required labeling elements included drug name, concentration, preparation date and time, participant’s initials, and expiration date and time. An error was identified if a required labeling element was either incorrectly recorded or illegible.
though clinicians were familiar with the standard manual labeling method using tape label rolls and a pen, they were not familiar with the new bar code-assisted labeling system. A brief, one minute overview of the new labeling system was presented to the clinicians. However, they did not have an opportunity to practice using the new system prior to their participation in our study.
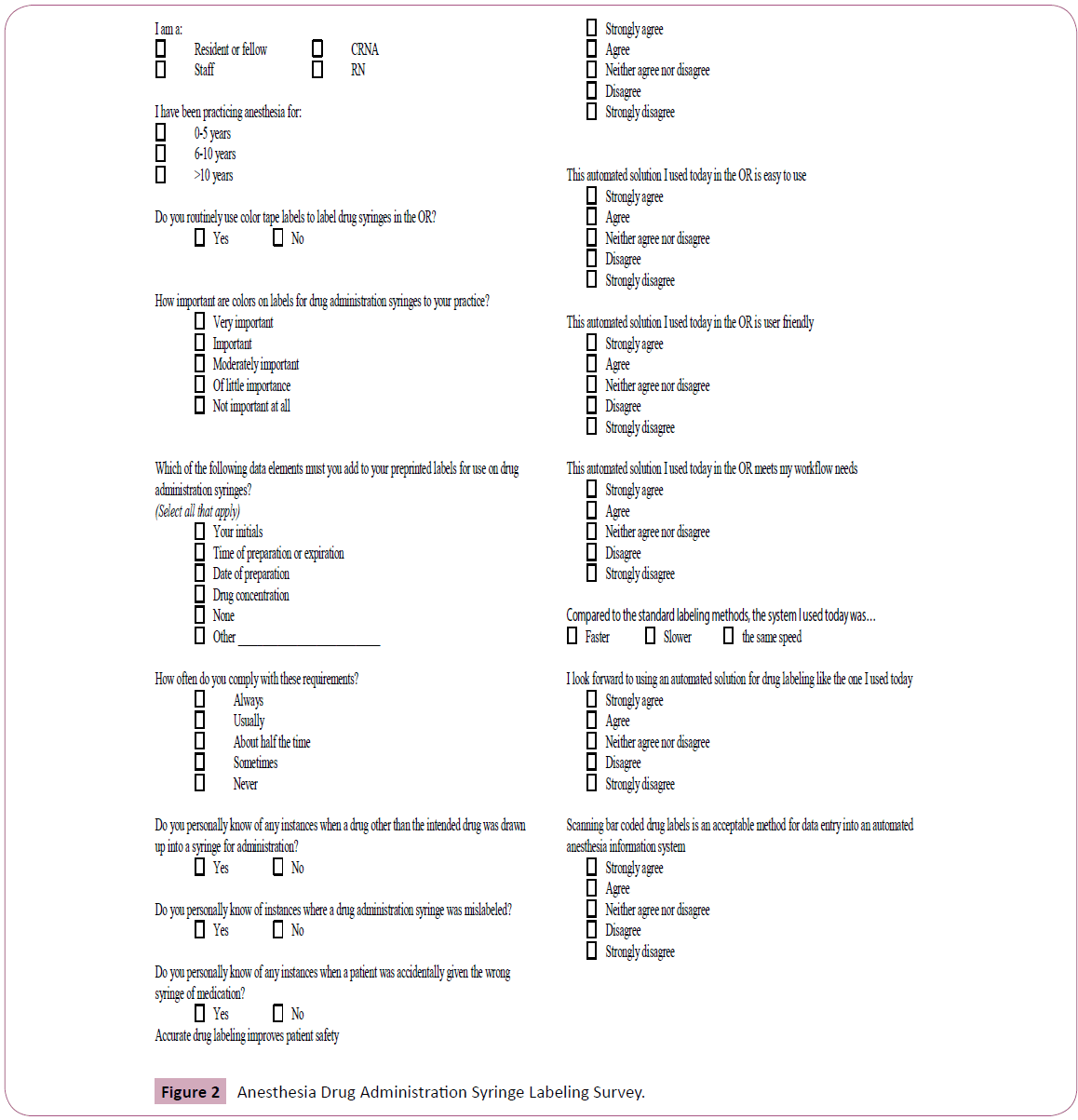
After using the bar code-assisted medication labeling system in our study, subjects were asked to complete a survey about their experiences using the system. The survey included information on participant’s demographics, current labeling practices, and previous medication errors, opinions on the relationship between labeling and medication errors, and satisfaction with the bar code-assisted syringe labeling system (Figure 2).
Statistical Analysis
Using a paired t-test, we assessed the difference in time taken for each subject to prepare medications using the bar code-assisted syringe labeling system and the conventional manual method. A p value of <0.05 was considered statistically significant. All calculations were performed using STATA/IC v10 (StataCorp LP, College Station, TX). For both data collection and analysis, we used one significant digit. We analyzed the survey data by calculating mean values for each likert scale response.
Results
Of 220 anesthesia clinicians at our institution, 64 volunteered to participate and were included in the study. Of the 64 participants, 28 (44%) were attending anesthesiologists, 27 (42%) were either residents or fellows and 9 (14%) were CRNAs. Each participant prepared three drugs (Succinylcholine, Propofol and Atropine) using both the conventional manual labeling method and the bar code-assisted syringe labeling system. A total of 192 syringes were prepared using each method. Total time to prepare the three medications was shorter using the bar code-assisted system (129.9s vs. 138.6s, p=0.01). Although the total time was shorter, the time taken to draw up Succinylcholine (43.7s vs. 44.6s, p=0.37) and Atropine (38.2s vs. 41.4s, p=0.12) using the bar code-assisted system was not statistically different from using the manual labeling method. The bar code-assisted method was statistically significantly faster for Propofol (50.0s vs. 56.6s, p=0.007).
Using the manual syringe labeling method, compliance with JC labeling requirements was lowest for expiration date/time (0.0%), followed by concentration (74.5%), time of preparation (75.0%), initials (80.7%) and date of preparation (88.0%), as shown in Table 1. As none of the syringes were labeled with the expiration date or time, overall compliance was 0.0% with JC labeling requirements. Excluding expiration date and time, 82 syringes (40%) were not compliant with the remaining JC labeling requirements. On average, syringes were noncompliant on 4 required data elements. Compliance with JC labeling requirements was 100% using the bar code-assisted syringe labeling system.
| Drug Name | Concentration | Date | Time | Initials | Expiration Date/Time | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | |||
| Bar code-assisted method compliance | 192 | 100.0% | 192 | 100% | 192 | 100% | 192 | 100% | 192 | 100% | 192 | 100% | 192 | |
| Manual Method | Compliance | 190 | 99.0% | 139 | 72.4% | 165 | 85.9% | 139 | 72.4% | 150 | 78.1% | 0 | 0.0% | 0 |
| Element Absent | 2 | 1.0% | 33 | 17.2% | 22 | 11.5% | 45 | 23.4% | 37 | 19.3% | 192 | 100.0% | 192 | |
| Element Illegible | 0 | 0.0% | 4 | 2.1% | 4 | 2.1% | 5 | 2.6% | 5 | 2.6% | 0 | 0.0% | 18 | |
| Element Incorrect | 0 | 0.0% | 16 | 8.3% | 1 | 0.5% | 3 | 1.6% | 0 | 0.0% | 0 | 0.0% | 20 | |
| Element Illegible or Incorrect | 0 | 0.0% | 20 | 10.4% | 5 | 2.6% | 8 | 4.2% | 5 | 2.6% | 0 | 0.0% | 38 | |
| Total Manual Method | 192 | 100% | 192 | 100% | 192 | 100% | 192 | 100% | 192 | 100% | 192 | 100% | ||
Table 1 Error rates and Compliance with JC-required Labeling Data Elements.
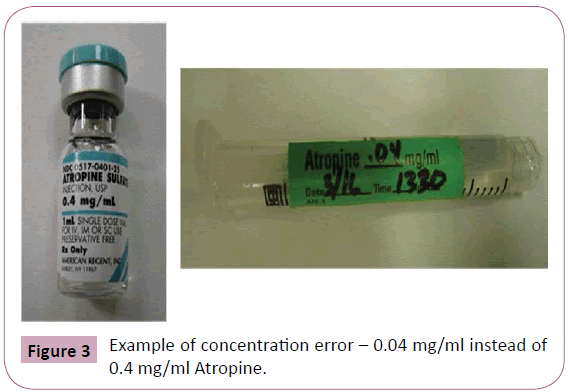
Of the 192 syringes prepared using the conventional method, we observed 38 errors on 24 syringes (Table 1). This corresponds to a 12.5% error rate, with erroneous labels containing an average of 1.6 errors. Of the 38 errors, 18 were illegible information and 20 were incorrect information. Incorrect drug concentration (Figure 3) accounted for 80% of incorrect information. No errors were found using the bar code-assisted system.
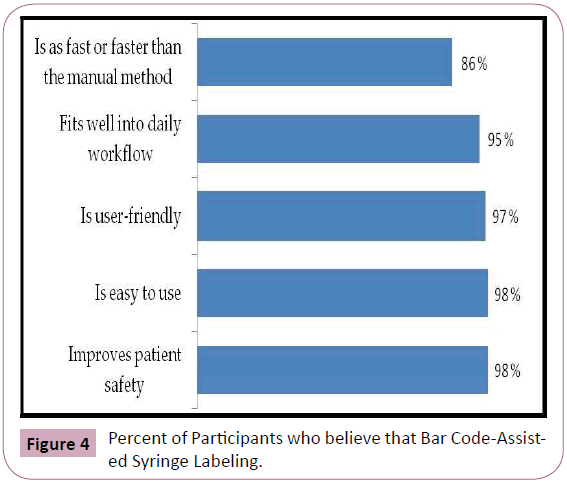
Analysis of the survey data (Figure 4) revealed that 86% of subjects perceived the bar code-assisted system to be as fast as or faster than the conventional method. 98% thought it improved patient safety, 98% thought it was easy to use, 97% thought it was user friendly, and 95% thought it fit well into their workflow.
Discussion
Bar code-assisted medication labeling not only ensured 100% compliance with JC medication labeling requirements but also eliminated labeling errors that were found with the conventional manual labeling method. The conventional manual method had a 12.5% error rate and 0% compliance with JC required labeling requirements. First time users found the system well integrated with clinical workflow, user friendly and easy to use. We expect that with some experience using the system, the time required for fully compliant syringe labeling will be reduced.
The literature supports our findings that anesthesia providers struggle with labeling compliance [4,9]. Furthermore, one in five hospitals receives a requirement for improvement from the Joint Commission related to medication labeling standards [10]. Noncompliance and labeling errors may be heightened with time pressure and emergent cases. Thus, bar code technology has the potential to improve perioperative patient safety and clinician communication, especially during handoffs, staff transitions and emergency cases.
Preparing medications using the bar code-assisted syringe labeling system was faster than using the manual method, even for first time users with minimal training, and this difference was statistically significant. However, the time difference was significant only for Propofol and not for Succinylcholine or Atropine. Potential explanations include the increased time required to draw up Propofol due to its high viscosity and increased volume. Furthermore, the amount of time saved is affected by when the medication vial is scanned during the drug preparation process, with maximum time saved when the vial is scanned at the start of the process, something not well known to the clinicians during the study. Succinylcholine and atropine are less viscous and require less time to draw up. Consequently, they might be drawn up before the bar code-assisted label is printed, especially if the vial is scanned part-way through the medication preparation process. While not all subgroups were significantly faster, they did all produce fully compliant and error free labels without slowing or impeding clinician workflow. The system’s ease of use and minimal perceived workflow disruption may facilitate its adoption. We did not attempt to optimize printer settings in our prototype system that may have also improved label printing speed.
We must recognize that the use and implementation of technology systems can be difficult and disruptive. Often workflow disruption and clinician dissatisfaction are cited as major reasons for failed technology implementation with the most public example being a computerized physician order entry system at Cedars-Sinai in Los Angeles that had to be withdrawn due to staff revolt even though it was properly functioning [11-14]. Technology systems alone cannot and will not prevent medication errors. Technology systems must be integrated with clinician workflow, standardization, workstation and workspace standardization, clear communication protocols and a strong safety culture [15].
The 2011 Joint Commission labeling guidelines allow hospitals to forgo the preparation date and time requirement for short procedures as defined by the hospital [8]. While this may help improve labeling compliance, it likely does not improve patient care. If clinicians do not know when a drug was prepared, it is impossible to determine the expiration date and time. Furthermore, drugs like Propofol that expire after six hr due to the risk of bacterial contamination should be clearly labeled with the preparation and expiration time in order to prevent dangerous medication errors, and these times are frequently missing. In addition, without the preparation and expiration dates and times, clinicians should discard and re-prepare all drugs at the time of each handoff. As anesthesia practice has evolved such that handoffs are commonplace during procedures, a lack of the date and time labeling requirement leads to a significant waste of drugs and clinician time.
Our study does have some limitations. First, participants knew they were being assessed and timed. Due to the Hawthorne effect, this knowledge may have improved their performance, such that actual compliance and error rates are even worse in daily clinical practice than what we observed [16]. Second, although the simulation was done in the operating room area with a realistic drug cart and working surface, it was not done in an actual operating room. This somewhat artificial setting may have also affected the participant’s performance. Third, all participants were anesthesia clinicians at a large academic tertiary care center, and the results may not fully generalize to clinician work patterns in other settings.
In summary, bar code-assisted syringe labeling is not only faster than conventional manual labeling methods but also ensures accuracy and compliance with JC labeling requirements. The improvement in labeling accuracy and compliance may reduce perioperative medication errors. This simple, innovative and inexpensive technology can be implemented with minimal effect on workflow. The adoption of bar code-assisted syringe labeling technology at other health care centers may achieve widespread improvements patient safety through the reduction of perioperative medication errors.
Financial Support
Funding received from the Department of Anesthesia, Critical Care and Pain Medicine, Massachusetts General Hospital; and The Sims Lab, Massachusetts General Hospital, Boston MA.
References
- Fasting S, Gisvold SE (2000) Adverse drug errors in anesthesia, and the impact of coloured syringe labels. Can J Anaesth 47: 1060-1067.
- Cooper JB, Newbower RS, Kitz RJ (1984) An analysis of major errors and equipment failures in anesthesia management: considerations for prevention and detection. Anesthesiology 60: 34-42.
- Webster CS, Merry AF, Larsson L, McGrath KA, Weller J (2001) The frequency and nature of drug administration error during anaesthesia. Anaesth Intensive Care 29: 494-500.
- Orser BA, Chen RJ, Yee DA (2001) Medication errors in anesthetic practice: a survey of 687 practitioners. Can J Anaesth 48: 139-146.
- Garnerin P, Perneger T, Chopard P, Arès M, Baalbaki R, et al. (2007) Drug selection errors in relation to medication labels: a simulation study. Anaesthesia 62: 1090-1094.
- Levine WC, Driscoll WD, Fishman G, (2008) "Smart Labels" - Improving Medication Safety in the Perioperative Environment. American Society of Anesthesiologists Meeting. Abstract A759.
- Guidance for Industry: Bar code label requirements questions and answers.
- Joint Commission Hospital National Patient Safety Goals 2011.
- Vernest K, Nanji KC, Driscoll WD, (2009) "Smart Labels": Improving labelling compliance and patient safety in the operating room. American Society ofAnesthesiologists Meeting. Abstract A609.
- [No authors listed] (2008) Top standards compliance issues for first half of 2007. JtCommPerspect 28:3.
- Neuenschwander M, Cohen MR, Vaida AJ, Patchett JA, Kelly J, et al. (2003) Practical guide to bar coding for patient medication safety. Am J Health Syst Pharm 60: 768-779.
- Miller RH, Sim I (2004) Physicians' use of electronic medical records: barriers and solutions. Health Aff (Millwood) 23: 116-126.
- Poon EG, Jha AK, Christino M, Honour MM, Fernandopulle R, et al. (2006) Assessing the level of healthcare information technology adoption in the United States: a snapshot. BMC Med Inform DecisMak 6: 1.
- Bates DW (2006) Invited commentary: The road to implementation of the electronic health record. Proc (BaylUniv Med Cent) 19: 311-312.
- Eichhorn JH (2010) Anesthesia Patient Safety Foundation Consensus Group Defines Challenges and Opportunities for Improved Practice. APSF Newsletter 25: 1-20.
- McCarney R, Warner J, Iliffe S, van Haselen R, Griffin M, et al. (2007) The Hawthorne Effect: a randomised, controlled trial. BMC Med Res Methodol 7: 30.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences